Table of Contents
- Introduction to Ischemic Stroke
- Characteristics and Types of Ischemic Stroke
- Thrombotic Stroke Definition
- Embolic Stroke Definition
- Other Categories of Ischemic Stroke
- Ischemia Mechanisms of Injury and Neuronal Cell Death
- Reperfusion and Spontaneous Reperfusion
- Size and Magnitude of Human Ischemic Strokes
- Technology Commonly Used to Induce Ischemic Stroke
- How to Choose the Right Animal Model for Ischemic Stroke Research
- Animal Models of Focal Ischemic Stroke in Clinical Research
- The Intraluminal Suture MCAo Model
- Craniectomy Models and Direct Vessel Occlusion
- The Three-Vessel Occlusion Model
- Photothrombotic Stroke Model
- The Endothelin-1 Model of Ischemic Strokes
- Thromboembolic Clot Models of Embolic Strokes
- Microsphere and Macrosphere Models: Embolic Stroke Models
- Spontaneous Stroke Model
- Animal Models of Global Ischemic Stroke in Clinical Research
- Animal Models of Cerebral Venous Sinus Thrombosis
- How Different Mouse Strains Affect Ischemic Stroke Modeling
- Overview of Assessment Methods of Ischemic Brain Injury
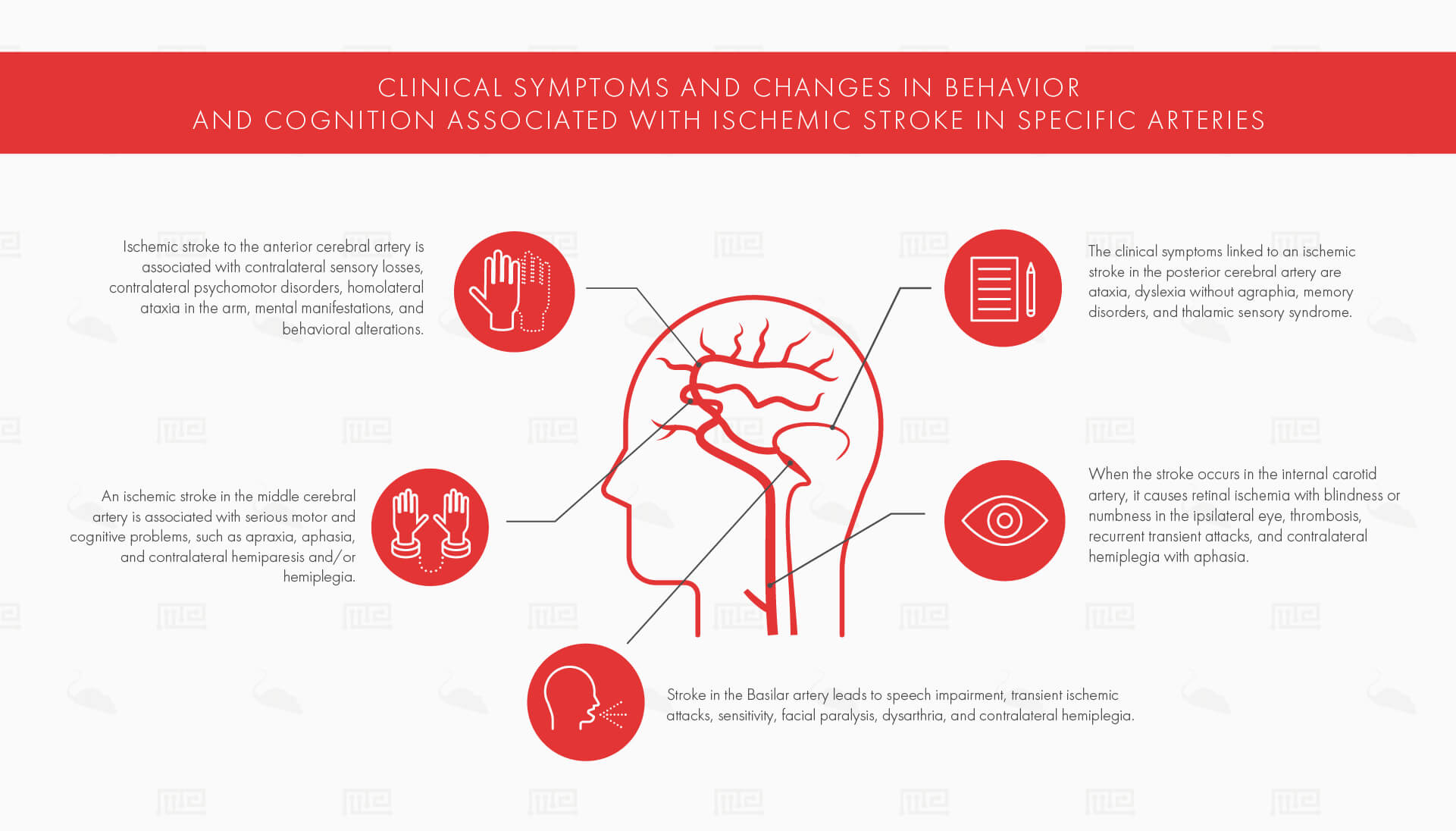
- The Major Human Arteries and Post-Stroke Clinical Symptoms
- Treatment Options for Ischemic Stroke
- Future Research
- References
Ischemic stroke is a serious, potentially life-threatening condition in which the brain experiences a sudden loss of blood supply to a particular brain region, leading to a subsequent loss of neurological functions. Unfortunately, there are no treatments which can help lead to a full recovery after ischemic strokes. In order to make progress, animal models are being used to in order to develop drugs, identify neuroprotective factors which may decrease post-stroke disability, and create effective therapeutic interventions.
In this article, we will discuss ischemic stroke, the relevant pathophysiology, reperfusion, and the factors which cause stroke. These topics are crucial to understand, prior to delving into ischemic stroke animal models, since so much of the success of animal models hinges upon appropriate representation of human stroke.
Then, we will review the most commonly used ischemic stroke animal models in scientific research and conclude with relevant techniques for acquiring research data in animal research. So, let’s get started!
Introduction to Ischemic Stroke
Ischemic stroke is a particular type of stroke. It is also commonly referred to as brain or cerebral ischemia. Brain ischemia is when the brain has insufficient blood flow to the brain. Thus, it cannot meet its metabolic demands, leading to low oxygen supply and cerebral hypoxia.
About 87% of all strokes are ischemic strokes. So, the inadequate blood supply to the brain is a clinical condition that is challenging doctors and researchers.
Ischemic strokes are caused by:
- Thrombus ( a “blood clot” that forms in one of the body’s arteries or veins)
- Embolus (any unattached mass which moves in the bloodstream and can clog it)
A thrombus or embolus lodge or block a blood vessel and thus disrupt blood flow. Therefore, the brain regions that are supplied by the particular blood vessel are unable to receive the necessary oxygen and nutrients for meeting metabolic demands. Sustained loss of cerebral blood flow damages the brain and may eventually lead to permanent brain tissue damage and, ultimately, death.
Characteristics and Types of Ischemic Stroke
As mentioned previously, ischemic strokes are caused by a thrombus or an embolus. Therefore, an ischemic stroke can be classified as either thrombotic or embolic. It is also possible to label an ischemic stroke as being either focal or global. So, depending on the cause (thrombus or embolus) and whether the ischemia globally or focally affects the brain, different outcomes will be observed and different interventions will be needed.
Thrombotic Stroke Definition
What is a Thrombus?
A thrombus is formed by red blood cells, aggregated platelets, and cross-linked fibrin protein. It results from blood coagulation, a step in hemostasis, and serves to create a seal in the blood vessel in order to prevent further bleeding resulting from injury. Therefore, a thrombus can be considered as a normal, healthy response to an injury.
It becomes dangerous and harmful when it obstructs the blood flow moving through blood vessels.
Thrombotic Stroke Types and Composition
- Large-vessel Thrombosis. An ischemic thrombotic stroke which affects the brain’s large blood-supplying arteries, such as the middle cerebral or carotid arteries.
- Small-vessel Thrombosis. A blockage which occurs in the smaller blood vessels that are located more deeply in the brain. Small-vessel thrombosis is oftentimes referred to as a lacunar stroke.
Furthermore, thrombi are described and classified based on the number of red blood cells and platelets that they are comprised of. The three groups for thrombi classification are:
- Red thrombi. Mostly composed of red blood cells.
- White thrombi. Predominantly made up of platelets.
- Mixed thrombi. An intermediate mixture containing both red and white thrombi.
Thrombus formation can occur due to:
- Abnormal blood flow
- Hypercoagulability
- Endothelial injury
In order for a model to be accurate, one of the first things it must do is reflect and resemble the composition of a naturally occurring thrombus. Due to these many factors which influence the nature of the thrombus, modeling thrombotic stroke in rodents can be challenging and is still a research area that is developing.
Venous Thrombosis Stroke
Venous thrombosis or cerebral venous sinus thrombosis is a type of thrombotic stroke which is caused by a blood clot that develops in the dural venous sinuses (responsible for draining the blood from the brain). This type of stroke is most likely to have a hemorrhagic transformation and have an accompanied blood leak into the affected area.[1]
Embolic Stroke Definition
An ischemic stroke can also be caused by an embolus. An embolus is a general term which refers to any mass which travels through blood vessels and, somewhere along the way, clogs the blood vessel due to its size.
Common types of embolisms which are encountered in clinical practice are:
- Fat embolism (created by fat droplets, typically from leaking tubular bones like the femur)
- Cholesterol embolism (created by cholesterol, also known as an atheroembolism)
- Thromboembolism (an embolus from a broken off blood clot, e. a thrombus)
- Air embolism (also referred to as a gas embolism or, in layman’s terms, a “bubble”)
- Cancer cells (metastasizing and moving to other parts of the body)
- Lumps of bacteria (such as those from endocarditis)
- Amniotic fluid embolism (where amniotic fluid or debris such as hair or foetal cells enter the mother’s bloodstream through the placenta)
Other Categories of Ischemic Stroke
Ischemic strokes can also be described or categorized based on how much of the brain is affected by the blockage.
- Focal Ischemic Stroke. A focal ischemic stroke occurs when one of the brain’s cerebral arteries is occluded (blocked). Therefore, a focal stroke affects a specific region and may impair the functions which that specific region is associated with.
- Multifocal Ischemic Stroke. A multifocal ischemic stroke is characterized by a patchy pattern, affecting multiple small vessels, of reduced cerebral blood flow. Multifocal ischemic stroke can be associated with other clinical conditions such as metastatic tumors.[2]
- Global Ischemic Stroke. Global ischemia, on the other hand, occurs because the cerebral blood flow is reduced throughout the majority (or all) of the brain.
Other pre-existing conditions or complications can cause a global ischemic stroke to occur. For example, when cardiac arrest occurs, the brain is also affected due to the subsequent decrease in circulating blood.[3]
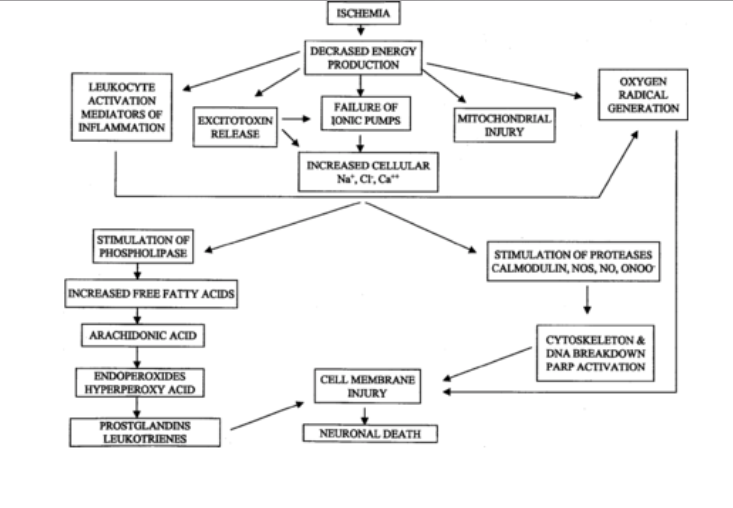
Ischemia Mechanisms of Injury and Neuronal Cell Death
One of the major goals of research which uses animal models of ischemic stroke is to establish the mechanisms of injury and neuronal cell death for the purposes of developing targeted and focused interventions, and therapeutic compounds.
In order to have animal models which accurately reflect ischemic
stroke, the pathophysiology between rodent models and human ischemic stroke must be similar. Therefore, understanding and capturing the pathophysiological process of human stroke is essential for developing animal models and advancing current knowledge.
When ischemia first develops, the area that has reduced blood supply is unable to meet its energetic demands. Since energy cannot be delivered to the neurons and brain cells, adenosine triphosphate (ATP) levels drop to suboptimal concentrations. When ATP levels decrease, lactate acidosis develops and the neurons’ ionic homeostasis becomes compromised.
With the loss of ionic homeostasis, neurotransmitters become affected. Glutamate, the primary excitatory neurotransmitter in the human brain, is commonly studied in ischemic stroke research. Glutamate is implicated in creating a large influx of calcium by binding with N-Methyl-D-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors. An increase of calcium concentration leads to activation of proteases and phospholipases which break down vital cellular proteins and membranes. Also, glutamate receptors are implicated in numerous pathophysiological cascades that occur during ischemic stroke, including the excessive influx of water and sodium which occurs in parallel with cellular swelling, the decrease of extracellular space, and edema.
During brain ischemia, due to high levels of sodium, calcium, and adenosine diphosphate (ADP), mitochondria are implicated in excessive free radical production. This toxic mechanism damages carbohydrates, proteins, lipids, and nucleic acids by activating apoptosis-related signaling such as the cytochrome c pathway.[4]
While these injury processes are occurring, cortical spreading depression is also unraveling due to the high extracellular concentration of K+. Cortical spreading depression is characterized by a sustained depolarization of glial and neuronal cellular membranes, loss of ion gradients and electrical activity, distortion of dendritic spines, and neuronal swelling.
The basic injury mechanisms which occur during brain ischemia are excitotoxicity (excessive glutamate activity), oxidative stress, vascular damage, inflammatory responses, apoptosis (programmed cell death), and damage to white matter and mitochondria. However, these are just a few of the major characteristics of ischemic stroke pathophysiology. A more detailed and comprehensive review is available here.
Reperfusion and Spontaneous Reperfusion
Reperfusion is whenever blood flow is restored to a tissue. Reperfusion is the goal of interventions, in order to resupply the tissue with blood.
Currently, spontaneous reperfusion is becoming a topic of scientific interest, a phenomenon in which the brain reperfuses on its own. Research papers that are being released estimate that about 15-18.8% of all strokes have early clot lysis as established by serial monitoring.[5] An embolic clot is more likely to recanalize spontaneously than a local thrombotic. Furthermore, clot and clots in the middle cerebral arteries are more likely to reopen spontaneously than clots in the internal carotid artery.[6]
Animal models can be used to study the effect of reperfusion. Models such as the intraluminal model (to be discussed in greater detail below) have been developed in such a way so as to make reperfusion possible. When the desired amount of time has passed after ischemic stroke induction, reperfusion is established by removing the object (such as a clip or a suture) which was previously inserted to create the occlusion (blockage).[7]
Size and Magnitude of Human Ischemic Strokes
Human strokes are typically small in their size. Large-scale population studies and clinical trials have demonstrated that strokes will range from 28-80 mm3. Translating this with human hemisphere volumetric measurements, such a stroke size is about 4.5-14% of the ipsilateral hemisphere.[5]
When a stroke is larger than 39% of the ipsilateral hemisphere, a malignant infarction will occur. For this type of stroke, medical therapy is basically ineffective and severe brain damage and even death will occur. About 10% of all strokes are classified as being a malignant infarction.
Technology Commonly Used To Induce Ischemic Stroke
In order to induce an ischemic stroke in rodents, technology is typically used. For example, after performing a craniotomy and opening the skull, the blood vessel can be occluded by:
- Surgical clips[8][9]
- Nylon thread, as is the case with the intraluminal filament model[10]
- Internal sealing via a photothrombotic lesion by using light and rose bengal dye[11]
How to Choose the Right Animal Model for Ischemic Stroke Research
Due to the large need for finding stroke interventions and therapeutic treatments, a large number of animal models of ischemic stroke have been developed and proposed. There are so many models to pick from, in fact, that it can get intimidating or overwhelming for a scientist to decide where to begin. Therefore, it is important to keep some criteria in mind, in order to make the most informed decision when it comes to picking the right animal model
Commonly used criteria for choosing animal models to conduct clinical research include the following:
- A reproducible ischemic lesion size
- The technique or method employed for inducing the model ought to be minimally invasive and easy to perform
- The pathophysiological responses which occur as a result of the induced ischemic stroke should resemble those found in human stroke
- The rodents’ brain samples should be used, in order to perform biochemical and histopathological assessments
- The model should be cost effective[12]
With these points in mind, model selection can be carried out purposefully. With an appropriate model selected, possible interventions and findings pertaining to cerebral ischemia can be uncovered.
Animal Models of Focal Ischemic Stroke in Clinical Research
Focal ischemic stroke, as mentioned previously, is a stroke wherein a specific blood vessel is blocked leading to ischemia in the brain region which would under normal conditions receive blood flow from the occluded vessel. In order for animal models to be useful and relevant, human ischemic strokes must be represented accurately. The next few sections will cover frequently used animal models and their advantages and disadvantages.
The Intraluminal Suture MCAo Model
The intraluminal suture model also referred to as the “intraluminal filament model” or the “endovascular suture model,” uses a thread to create a middle cerebral artery occlusion (MCAo). The MCAo model is currently the most popular rodent model used in ischemic stroke research. Some researchers even refer to it as “the gold standard for mechanistic studies.”[10] In fact, it has been used in approximately more than 40% of the 2,600+ experiments which have been conducted to study post-ischemic stroke neuroprotection.[13]
General Protocol for the Intraluminal Suture MCAo Model
This model requires the use of a nylon thread, introducing it into the internal carotid artery and moving it upwards until it blocks the origin of the middle cerebral artery. In more detail, the common carotid artery is temporarily occluded, then a suture is introduced into the internal carotid artery and it is moved upwards until it interrupts the middle cerebral artery’s blood flow.
It is also possible, in a modified version, to insert the suture into the external carotid artery and advance it until it reaches the inner carotid artery and eventually the middle carotid artery. This procedure is typically monitored by the simultaneous use of laser Doppler flowmetry (LDF) which measures the rodent’s relative cortical perfusion, thus ensuring that the model is induced successfully.[14][15]
The MCAo model is commonly used in rodents, both mice and rats, and was first proposed by Koizumi and colleagues based on their conducted research utilizing rats. Since then, the model has gone through multiple modifications with regards to the filament’s coating and length.
Studying Reperfusion with the MCAo Model
The intraluminal suture model can model permanent ischemia or transient/temporary ischemia (as determined by the withdrawal of the suture and the subsequent reperfusion) across various time points. So, it is advantageous in the sense that it offers both a permanent and a transient ischemic model. If the topic of study is transient ischemia with reperfusion, then it is best to induce MCAo via the external carotid artery because it maintains the vessels’ anatomical integrity which is necessary for successful reperfusion.
Reperfusion can be closely studied with this model. Typical intervals of stroke duration are 60, 90, and 120 minutes (prior to reperfusion), or permanent occlusion. The success rate associated with MCAo is 88%-100%.[14] So, such a high success rate is obviously a major advantage. But, when inducing MCAo there is a 12% risk of a subarachnoid hemorrhage to occur.[16] These approximations are similar in rats and mice.
By stalling reperfusion, neuronal death or pannecrosis in the ipsilateral hemisphere will occur. The striatum is affected in MCAo in Wistar rats, as are the frontoparietal and temporal cortices, some areas of the occipital cortex, the hypothalamus, and thalamus. When MCAo occurs via the intraluminal suture model, the striatum experiences early ischemia and, eventually, the cortex on top of the striatum will be infarcted, too.[17]
Using the MCAo Model to Study Stroke Ischemia Interventions
Since the MCAo is such a commonly used ischemic stroke model, it is frequently used in order to study how interventions, such as supplementations with neuroprotective properties, can affect post-stroke outcome and functionality.
For example, one study set out to examine how melatonin would affect behavior in C57BL6/J mice that had an ischemic stroke-induced via an MCAo which lasted for 30 minutes. After induction, some of the mice were given melatonin for the course of 29 days and the rest served as controls.[18] The treated mice had improved performance in the Grip Test and lower anxiety levels in the Open Field Test when compared to the untreated controls. Such a study demonstrates how MCAo is used in research.
Advantages of the Intraluminal Suture Model
- Reflects the location of stroke as found in humans. Since this model is localized to the middle cerebral artery which is also the major stroke site in humans, this similarity serves as an advantage.
- Creates blood-brain barrier injury. Thus, therapeutic techniques can be developed to target this.
- Initiates inflammatory processes and cell death pathways.
- Does not require a craniectomy to induce. Therefore, it does not run the risk of damaging other cranial structures as a result of the surgical process.
- Creates a penumbra. A penumbra (the neuronal tissue which surrounds the infarct but has not yet been irreversibly damaged) which is commonly observed in humans that have had an ischemic stroke should always be represented by an animal model.
- Causes cognitive problems which resemble those found in humans. Humans tend to develop memory problems after stroke,[19] an impairment which also develops in rats after MCAo induced stroke as established by studies utilizing the Morris Water Maze.[20] [21]
Disadvantages of the Intraluminal Suture Model
- Elicits some symptoms not found in human population. After the middle cerebral artery has been occluded in rats for 120 minutes or more, the hypothalamus gets affected, leading to spontaneous hyperthermia in rats.[22] In mice, this model can lead to hypothermia.[23] In human ischemic stroke, hypothermia and hyperthermia do not occur after the middle cerebral artery has been occluded.
- Requires anesthesia to induce. Use of anesthesia can serve as a confounding variable in experimental results.
- Creates large infarcts. Large infarcts are more characteristic of a malignant infarction than of focal ischemic stroke.
Creates prompt reperfusion. When the filament is withdrawn, the occlusion is reperfused quickly and promptly, a situation which does not mimic human conditions wherein reperfusion is more gradual.
Craniectomy Models and Direct Vessel Occlusion
Ischemic models can be created in rodents by directly occluding a blood vessel in the brain. These models enable reperfusion if induced by means of clipping, using hooks, or ligation. However, if cauterization is used with transection, permanent ischemia will result. These approaches have one thing in common: a craniectomy must be performed and an incision through the dura mater covering the outer layer of the brain must be made.
The two main techniques used to induce a craniectomy model are discussed below, offering their own sets of advantages and disadvantages.
The Zygomatic Arch
The first common craniectomy technique separates the temporalis muscle and the parotid gland, transecting the zygomatic arch, and then removing the part of the skull that is near the middle cerebral artery. MCAo can then be achieved using a variety of means, including electrocoagulation (which permanently blocks the vessel), hooks, a microaneurysm clip, or ligatures.
Neuropathological analysis has shown that inducing MCAo through the zygomatic arch affects the cortex and the basal ganglia which can be an advantage or disadvantage depending on the researcher’s hypothesis or area of interest.[24]
Advantages
- Focal and precise. Due to the level of precision associated with this technique, researchers can have a high level of control over the model.
- Can occlude MCAo. This method allows for the occlusion of MCAo which is an advantage since so much of ischemic stroke research is focused on this artery.
- Can be permanent or transient. After accessing the MCA, the researcher can choose whether they want to induce permanent or transient ischemia.
Disadvantages
- Requires a craniectomy. To do a craniectomy, a high level of surgical skill and knowledge is required. Thus this may be a disadvantage for research teams that are limited in resources.
- Location of arteries may be difficult. Due to anatomical variation across rodent strains, locating arteries may be challenging at first. So, it is recommended to run a pilot study first with the strain, in order to avoid any obstacles during the intervention study.
- Uses anesthesia. Anesthesia must be administered prior to running a craniectomy, thus may be potentially confounding to the results and observations acquired while using this model.
The Three-Vessel Occlusion Model
The three-vessel occlusion (3VO) model is the second option for inducing ischemic stroke via a craniectomy. In this approach, both of the common carotid arteries are blocked, in addition to the middle cerebral artery (and sometimes, alternatively, the basilar artery), causing a reduction in blood flow which leads to ischemic damage. The infarct size is dependent on whether the arteries are permanently or temporarily blocked.
Advantages
- Impairs specific brain regions. The 3VO craniectomy model will impair the frontal, temporal, parietal, and rostral occipital cortices, the white matter, and a portion of the striatum in Wistar rats.[25]
- Control over reperfusion schedule and infarct size. Offers control over the duration which the artery is occluded. Also, infarct size is controlled based on how long the artery was occluded.
- Less variability. The suture model has much higher variability in the infarct and lesion size it creates when compared to the 3VO model.[26]
- Avoids the damage which the suture MCAo model creates. This method does not create undesirable damage to the hippocampus, midbrain, thalamus, and hypothalamus as the MCAo suture model does.
Disadvantages
- Requires a craniectomy. When performing a craniectomy intracranial pressure and the blood-brain barrier will be affected, therefore possibly influencing results. So, a high level of surgical skills will be required for inducing this model successfully.
- Uses anesthesia. The use of anesthesia may potentially confound the results.
General Advantages of Craniectomy Models
- Useful pathophysiology. Relevant inflammatory processes and cell death pathways can still be studied when using this animal model.
- Penumbra is present. Of importance, the penumbra is present in craniectomy models.
- Visual confirmation of MCAo. Researchers have immediate confirmation that the MCAo has occurred because they can see it happening.
- Reproducibility. Craniectomy models rank high in reproducibility of neurologic deficits and infarct size.
General Disadvantages of Craniectomy Models
- Must cut through the dura mater. This necessary step, cutting through the dura mater, is a major disadvantage because it does not reflect the reality of human stroke. Craniectomy, in fact, is more similar pathophysiologically to skull trauma (which shares its characteristics of inflammation and cortical spreading depressions).
- Risk of drill or thermal damage. Furthermore, a craniectomy may cause direct damage to the brain due to injury from the drill or thermal damage resulting from electrocoagulation of a blood vessel.
- Exposure to surrounding atmosphere. During a craniectomy, the brain is exposed to the surrounding atmosphere which may, in turn, may affect results by potentially altering the intracranial pressure and regional temperatures in the brain.
- May injure mastication muscles, if extracranial carotid artery is transected. If the extracranial carotid artery is transected during this model, the rodents’ mastication muscles will be affected, therefore causing difficulty in swallowing and eating, ultimately leading to weight loss. Such consequences affect behavioral outcome measures in post-stroke assessments, leading to poorer performance and serving as a confounding variable.
Photothrombotic Stroke Model
The photothrombotic stroke model also referred to as the photochemical stroke model, is typically used in rats but has modified protocols which are available for mice.
To induce stroke, a photoactive dye (rose bengal dye and erythrosin B are the most frequently used) is applied systemically. The photosensitive dye is injected intraperitoneally in mice or intravenously in rats.[27][28]
Using light with a specific wavelength, the brain is illuminated (the skull is still intact). The dye is activated by the illumination and subsequently, there is a formation of superoxide and singlet oxygen. This chemical reaction creates oxygen radicals which cause endothelial injury, platelet activation, and aggregation in the brain’s parenchyma and pial matter.
The “Ring Model” Modification of the Photothrombotic Model
Modifications of the photothrombotic model are underway, in hopes of making it mimic the human condition of ischemic stroke more closely. For example, the “ring model” uses a ring filter created by a circular laser beam.[29] This modification creates a central area that is thrombosis-free while the surrounding area is all damaged tissue. Therefore, the area in the middle is the penumbra, the tissue that is at risk of greater damage and is characterized by hypoperfusion.[30]
But, this modified model is still under scrutiny and assessment, in order to determine whether it truly and accurately reflects the penumbra which occurs in humans.
Advantages of the Photothrombotic Stroke Model
- High specificity and easily reproducible. By applying the activated light to the desired area based on precise stereotactic coordinates, an ischemic lesion can occur in the brain region of interest.
- Easy to control and manipulate. The depth and size of the ischemia in the photothrombotic model is controlled and varied via the photochemical dye and the light. By adjusting the dye’s plasma concentration or by altering the duration and intensity of light, ischemic damage is manipulated.
- Low mortality rate. Not many rodents will be lost to research when using this method, making it ideal for studying long-term functional outcomes and repair mechanisms after an ischemic stroke to a particular brain area.
Disadvantages of the Photothrombotic Stroke Model
- Does not reflect human stroke pathophysiology. While human ischemic stroke is defined by cytotoxic (intracellular) edema, the photothrombotic ischemic stroke model involves both cytotoxic and vascular (extracellular) edema combined with a rapid breakdown of the blood-brain barrier.[31]
- No penumbra. This model does not have a penumbra which is a major issue since a large interest of therapeutic interventions is to prevent permanent damage to this critical tissue.
- No reperfusion option. While the other methods can be either permanent or transient, the photothrombotic stroke model is resistant to reperfusion due to the nature of the lesion. Thus, it cannot be applied in research which seeks to establish therapeutic interventions for reperfusion.
Future Investigations and Additional Considerations
Furthermore, the entire photothrombotic model is being reconsidered by researchers questioning whether platelet activation actually plays such a major role in pathophysiology. Research is being conducted in order to determine whether “photothrombotic” may be a misnomer. So, this model, although is reproducible and specific, still needs future research in order to be fully grasped and understood.
Current Advancements of the Photothrombotic Model
Current developments of the photothrombotic model involve the use of stereotactically implanted optic fibers. Recent experiments have used this technique in order to induce an ischemic stroke affecting the internal capsule and the striatum.[32][33] This approach damages white matter and produces motor deficits.
Another development is a technique in which cerebral blood flow is monitored in real-time while inducing a photothrombotic stroke in freely moving, conscious rats.[34] Such advancements are promising because they permit for new realms of investigation to unravel.
One experiment, using implanted optic fibers, showed that within 25 minutes of activating the optic fibers to induce ischemia, performance in the Rotarod test is already comprised given detectable behavioral changes. The group that had ischemia had significantly different first latency to fall from the Rotarod test when compared to the non-ischemia group which had inactivated optical fibers.[35]
Such a technique can be combined with drug development research, in order to see how pharmaceutical intervention can affect motor and cognitive outcomes shortly after an ischemic stroke occurs.
The Endothelin-1 Model of Ischemic Strokes
Ischemic strokes induced by endothelin-1 in rodents are also commonly used in stroke research. Endothelin-1 is a peptide with vasoconstrictive properties that are long-lasting, effective, and potent.
Using Endothelin-1 Is to Induce Ischemic Stroke
To induce ischemic stroke, endothelin-1 can be used in many different ways. It can be:
- Applied to an exposed blood vessel[36]
- Stereotactically injected into the brain (which leads to vasoconstriction and therefore ischemia)[37]
- Applied directly on the brain’s surface[38]
The first two methods above lead to an ischemic lesion which is similar to the one created by MCAo.
When concentrations of endothelin-1 vary, different effects are produced. The concentration level determines the duration and severity of the subsequent ischemia and the infarct size. Endothelin-1 rapidly decreases cerebral blood flow (70%-90%) and has a reperfusion period which can last for several hours (until its effects wear off).
This model was initially developed in rats but has been modified in order to be used in mice.
Notably, endothelin-1 is about four times more powerful and potent in rats that are conscious than in rats subjected to anesthesia.[39]
Using Endothelin-1 to Induce White Matter Ischemia
Recent developments have used endothelin-1’s vasoconstrictive property in order to create a model that leads to white matter ischemia in the brain’s internal capsule and creates sensorimotor deficits.[40] Capturing ischemia localized to white matter is generally challenging because white matter does not receive as much blood flow as gray matter does.
Using Endothelin-1 for Anterior Cerebral Artery Occlusion
Endothelin-1 can induce anterior cerebral artery occlusion bilaterally when stereotaxically injected.
One experiment that was assessing ischemia via endothelin-1 occlusion of the anterior cerebral arteries demonstrated that the ischemia is localized to the anteromedial basal forebrain and medial prefrontal cortex. Due to the damage of these frontal areas, executive impairments were subsequently noted.[41] Damage to these regions in Lister hooded rats was associated with difficulties in selecting and initiating responses as demonstrated in their performance in the nine-hole box apparatus when compared with rats that did not have the anterior cerebral artery occluded bilaterally.
Also, endothelin-1 induced ischemic stroke models create motor disabilities. One study demonstrated using the Horizontal Ladder (wherein mice are expected to walk symmetrically across a ladder with evenly spaced distances between its rungs) that the C57BL/6 mice which had an ischemic stroke due to endothelin-1 exposure had significantly higher contralesional errors when compared to the shams.[42]
Advantages of the Endothelin-1 Models
- Flexibility. Virtually any region of the brain can be targeted and manipulated by the endothelin-1 technique. It can target deep regions of the brain as well as those which are more close to the skull.
- Models lacunar stroke. Lacunar stroke (the ischemic stroke which occurs in the brain’s smaller blood vessels) is easily modeled with endothelin-1.
- Long-term studies. Endothelin-1 is useful for long-term studies or experiments which aim to study the recovery mechanisms behind stroke.[43]
- Reperfusion characteristics are similar to humans’. When the effect of endothelin-1 ceases and wears off, blood flow will re-establish gradually, therefore resembling some cases of transient focal ischemic stroke (where the ischemia is not permanent).
- Low mortality. Not many rodents will be lost from this model, so using it will not be taxing on the laboratory’s resources.
Disadvantages of the Endothelin-1 Models
- Minimal edema present. Under this model, there is only minimal edema developed. So, it does not reflect human stroke exactly.
- Variations of batch potency. Since this model relies on the potency of endothelin-1, the chemical’s potency must be consistent from batch to batch, in order to avoid variability.
- Affects astrocytes and neurons. Endothelin-1, endothelin-1 receptors, and endothelin-1 converting enzymes are not just expressed by endothelial cells but also by neurons and astrocytes. So, injecting this vasoconstrictor will affect components of the brain in a way that does not occur in stroke.
- Induces astroglial prolificity. It has been demonstrated that the endothelin-1 application can induce prolificity in astroglia which in turn enables conditions for axonal sprouting. This increase in axonal sprouting may interfere somehow with post-stroke recovery and confound any additional findings.
Thromboembolic Clot Models of Embolic Stroke
Typically, in thromboembolic models, the clot is introduced either from thrombin-induced thrombotic material or is spontaneously formed, either from autologous or heterologous blood. Autologous blood is more commonly used for introducing clots than heterologous blood. Thrombin (a protease which is involved in forming fibrin during blood coagulation) may also be injected.
Based on the number or clots, the clots’ size, and the chosen application route, one or multiple blood vessels will be occluded thus causing infarcts in the brain regions which the occluded vessels are responsible for supplying blood to.
So, thrombi can be injected into extracranial arteries, in order to reach the intracranial arteries and cause ischemia. Due to the location where the injection is administered, a craniectomy is not required for this type of model.
After the clot has been injected it takes about 1 hour for the microvessels in the cortex to reopen. It takes 3 hours for the cortical vessels to be reperfused and about 24 hours for the striatal vessels.[44] These time estimates may vary slightly depending on the clot’s size and elasticity,[45] Researchers speculate that this is most likely due to the body’s endogenous thrombolysis mechanisms.[46]
To date, thromboembolic clot models have offered a sound base for analyzing and exploring therapies, leading to developments such as the recombinant tissue plasminogen activator (rtPA) which is the leading thrombolytic compound used in clinical practice.
Advantages of Thromboembolic Clot Models
- Reflects the most common type of stroke found in humans. In humans, thromboembolisms are the most common cause of cerebral ischemia. Therefore, thromboembolic clot models have the advantage of mimicking human stroke based on the fact that they reflect the leading cause.
- Resemblance to human pathophysiology. Embolic strokes in animals and humans are both primarily comprised of cytotoxic edema and later followed by vasogenic edema combined with the breakdown of the blood-brain barrier, including the presence of a penumbra, contain an inflammatory response, and spreading depressions.[47] Therefore, there is a close resemblance in the pathophysiology that occurs in reaction to the ischemic stroke.
- High potential for testing thrombolytic agents. Thromboembolic clot models are used to assess the ischemic area after it has undergone thrombolysis, and to examine how combination therapies (such as neuroprotective drugs combined with thrombolytic compounds) affect the outcome.
- Can be combined with MRI. The flexibility of this model has even extended to include application in real-time magnetic resonance imaging (MRI).[48][49]
Disadvantages of Thromboembolic Clot Models
- Variability. Large variability means that more rodents are needed to conduct the experiments, in order to reach statistical significance and meaningful results, and this can be taxing on the laboratory’s resources. The infarct volume in the thromboembolic model is still more variable than that of the MCAo.[49]
- Difficulty applying a control group. It is very challenging to have a control group when using this model since lesions cannot be consistent from mouse to mouse. One reason for this variability is uncontrollable reperfusion. Researchers cannot control the rate at which a blood vessel is reopened and thus cannot easily have a control group in which the rodents are all exposed to equally long ischemia.[10]
- Does not mimic clinical emboli. The thrombin injection would create a clot which is mostly comprised of fibrin (a composition profile which is not similar to the clots found in humans) and have low concentrations of platelets and cells.[50] By contrast, human clots have platelet/fibrin accumulation, erythrocytes, and neutrophil/monocytes.[51]
- High mortality rates. Embolic models are associated with higher mortality rates (for rats, 30% and greater)
- Likelihood of hemorrhaging. With this model, hemorrhaging is also likely to occur which is a factor that complicates experiments.
Microsphere and Macrosphere Models: Embolic Stroke Models
Just like thromboembolic stroke model, microsphere and macrosphere models aim to mimic embolic stroke. But, instead of using blood clots or thrombin to create an occlusion (as is the case in thromboembolic stroke models) these models make use of non-organic objects like little metallic balls.
Microsphere Models
Spheres that have a diameter of 20-50 μm are utilized in microsphere models. Commonly used materials for this model are a superparamagnetic iron oxide, dextran, ceramic, and TiO2.[47]
These microspheres are inserted into the internal carotid artery or the middle cerebral artery via the external carotid artery. A microcatheter is inserted into the external carotid artery and then the microspheres are passively introduced into the cerebral circulation.
The microsphere model ranges in severity and impact based on the size and amount of the microspheres that are used during experimentation.[52] Since animals generally have a good tolerance for microembolization, sometimes large amounts of microspheres are injected, in order to affect the cerebral vasculature.
The microsphere model is characterized by a lesion size that grows slowly and steadily up to the 24 hour period post-injection and may continue up to the 48 hour time point. By comparison to the MCAo model, the microsphere model’s lesion development rate is much slower.[53]
Microsphere models, since they are non-clot emboli, are permanent and cannot be disintegrated, so interventional and spontaneous recanalization of blood cannot occur. These limitations are a slight disadvantage as they limit the utility and application of microsphere models.
Microsphere Models Using Cholesterol Crystals
Recent advancements in microsphere models have steered in the direction of using small compounds which are frequently implicated in embolic strokes.
For example, cholesterol crystals are being used to study microemboli which occur in asymptomatic carotid atherosclerosis.[54] In this model, cholesterol embolization is associated with an inflammatory reaction and the activation of astrocytes and microglia. Furthermore, while the level of neuronal injury is low, animals will still show cognitive impairments after receiving multiple injections.
In one experiment using this type of embolic stroke model, four weeks after the cholesterol crystals were injected, behavioral testing revealed significant differences between controls and rats under this model. When compared to the sham-operated rats, the embolic rats exhibited anxiety-like behaviors and significant impairments in motor learning.[54] The embolic rats performed worse than control on Day 5 of the Barnes Maze, indicating weaker memory abilities. The embolic rats made more errors in finding the escape hole and employed a more random searching strategy for the escape route while the controls were more direct when completing the task. In the Open Field Test, on Day 1 after the stroke was induced, the embolic rats also showed more preference for the corner areas and avoided the center of the maze more than the control group did.
Macrosphere Models
In the macrosphere models of embolic stroke, the spheres that are used are larger than those in the microsphere models, thus differentiating in terms of diameter.
Macrosphere models make use of spheres ranging from 100-400 μm in diameter. These macrospheres are introduced to the cerebral blood flow via the internal carotid artery wherein they create focal ischemic lesions similar to those created during MCAo model induction.
Unlike the MCAo model, the macrosphere model does not produce ischemia to the hypothalamus and thus hyperthermia does not develop in the experimental rats.[55]
The macrosphere model is useful for studies seeking to examine neuroprotective therapies. Also, it can be applied to stroke research aiming to examine ischemia under challenging conditions, such as inside an MRI scanner or in awake rodents.
Spontaneous Stroke Model
Spontaneous stroke models were developed over 50 years ago by Okamoto and Aoki, and are induced using a specific type of animal.[56] The rats that are used to induce this model are the:
- Spontaneously hypertensive rat (which is a selectively inbred from the Wistar-Kyoto rats)
- Stroke-prone spontaneously hypertensive rat (which is a substrain of the spontaneously hypertensive rat)
Given that hypertension is the top modifiable risk factor in humans when it comes to stroke, spontaneous stroke models make use of hypertensive animals in order to mimic clinical reality.
The spontaneously hypertensive rat is born normotensive and by 2 to 4 months of age develops hypertension due to an overly active renin-angiotensin system. By 6 months of age, this rat will have high blood pressure with a systolic value of approximately 200 mmHg. This rat does not develop stroke but is used as the basis for inducing other types of stroke models.
The stroke-prone spontaneously hypertensive rat, when given a high-salt diet, will develop hypertension when it is just 6 weeks old. Continuing on this diet, by 12 weeks of age, it will begin developing malignant hypertension (>240 mmHg). Then, by 20 weeks of age, cortical strokes combined with hemorrhages in the occipital, parietal, and frontal regions of the brain will already appear.[57]
By using rats that reflect the risk factors in humans for developing ischemic stroke, preventative or neuroprotective agents and interventions can be developed which are specific to these mice and phenotype.
Advantages of Spontaneous Stroke Models
- Reflects clinical reality. By using spontaneously hypertensive rats, this model replicates clinical reality by representing one of the human phenotypes that is highly at risk of having an ischemic stroke.
- Develops small vessel disease. The hypertensive small vessel disease which occurs in this model causes small infarcts are known to develop in the subcortical white matter and striatum of the brain. Such characteristics offer a useful context for research to be conducted.
- Similar pathophysiology to humans. Furthermore, small vessel disease is linked to fibrinoid necrosis, arteriolar wall thickening, and perivascular space enlargement. Such features are similar in humans.[58]
Disadvantages of Spontaneous Stroke Models
- Difficulties in translating subsequent findings. Since spontaneity is a key feature of the spontaneous stroke model, the moment that the stroke will occur is unpredictable. So, it is quite challenging for the researchers to determine and attribute which behavioral and cognitive changes were caused by the stroke and which changes are a reaction to the stroke.[22]
- Lack of control. As mentioned previously, this model is characterized by its spontaneity. Therefore, it is incredibly difficult to create controls groups and control for infarct size and duration.
Future Directions of Spontaneous Stroke Models
Spontaneous stroke models, due to their similar pathophysiological similarity with humans, will continue to develop. For example, current research is working on expanding the repertoire of rodents available for inducing this model. Male inducible hypertensive rats or the (R+/A+) mice are also being studied for their ability to develop spontaneous ischemic and hemorrhagic strokes after being restricted to a certain diet.[59]
Global Ischemic Stroke Animal Models in Clinical Research
Global ischemic strokes, as mentioned previously, create ischemia which affects the entire brain. Instead of the ischemia being localized to a specific vessel and affecting a certain region, global ischemia impacts the entire brain due to globally reduced blood flow.
When the blood flow occlusion is still limited in time, global ischemia specifically creates neuronal injury in the hippocampus’ CA1 region. As time progresses and the duration of the ischemia extends and other brain regions become affected. In global ischemic stroke, when blood flow restoration is unsuccessful, it is known as the “no-reflow phenomenon.”
Commonly used global ischemic stroke animal models also utilize the circulatory system, since global ischemia frequently occurs as a result of a failed circulatory system. Global ischemic stroke animal models are typically studied in large animals, such as pigs and dogs since mouse models of global ischemia usually resulted in creating seizures and a high mortality rate. However, developments, efforts, and modifications have been made in order to make global ischemia more easy to model in rodents.
Four-Vessel Occlusion Method
In the four-vessel occlusion (4VO) model, the common carotid arteries and the vertebral arteries are reversibly occluded, thus four vessels are occluded in total.[60] Permanent occlusion of the vertebral arteries by means of electrocauterization is also possible. These combined techniques cause ischemia bilaterally to the forebrain and brainstem.
The brain damage which occurs under 4VO most closely resembles the damage in humans which is observed after cardiac arrest. Selective neuronal death occurs and the astrocytes undergo hypertrophy in the ischemic core.
Confirmation of the model and ischemia is acquired during a neurobehavioral assessment. Rodents are grouped based on the severity of behavioral deficits, such as losing the righting reflex. Once the examination is complete, then the interventions and experiments begin.
Advantages of the 4VO Model
- Predictable brain damage. In rats, the most frequently damaged brain areas resulting from this model are the paramedian and H1 hippocampus, the striatum, and the posterior neocortex (layers 3,5, and 6).[61]
- Low seizure incidence. Seizures are not likely to occur in this model.
- No use of anesthesia. Anesthesia cannot act as a potential confounding variable as in models which use it. In fact, this model can be induced in freely moving animals.[3]
- Easy protocol. This model is easy to maneuver when working with many rodents.
- Reflects damage found in humans. This model appropriately reflects the damage found in humans after going through cardiac arrest.
Disadvantages of the 4VO Model
- Controversial cell death mechanisms. The cell death mechanism that occurs in 4VO is still unclear and controversial, with disputes occurring as to whether there are distinct characteristics of apoptosis or necrosis or both.
- Only specific strains can be used. Research using the 4VO model is usually limited to the Wistar rat strain, in order to successfully induce ischemia and avoid high mortality rates.[62]
- Variability of ischemia. Since the ischemia cannot be visually confirmed,
- Use of anesthesia. Although the original protocol developed for 4VO in 1979 did not use anesthesia, contemporary modifications may use anesthesia.
Two-Vessel Occlusion Method
The two-vessel occlusion (2VO) method is used as an alternative to the four-vessel occlusion method. In the two-vessel occlusion method, global ischemia is induced by blocking the two common carotid arteries only while inducing temporary hypotension, as defined by a mean pressure of 50 mmHg.
The two-vessel occlusion method induces nearly total ischemia while post-ischemic recovery is heavily dependent on the residual flow rates.
This model is characterized by selective neuronal vulnerability, affecting hippocampal CA1 pyramidal neurons, the dorsoventral striatal neurons, and the neocortex’s pyramidal neurons in layers 3 and 4.[63]
Advantages of the 2VO Model
- Temporary ischemia. Due to the reversibility of the ischemia, this model can be used in order to perform long-term recovery studies.[64]
- Consistent brain injury. The 2VO model is associated with consistent injury to the following brain regions: the caudate putamen, the hippocampus’ CA1 region, and the neocortex in rats. So, researchers can pick this model if they are interested in studying these brain regions.
- High reproducibility. The reproducibility of the ischemic damage caused by this model is estimated to be more than 90%.[63]
- Flexibility in application. The 2VO model can be used for physiological and biochemical studies, as well as for assessing neuroprotective agents and interventions.
Disadvantages of the 2VO Model
- Short timeframe for action. After 10 minutes of ischemia under this model, permanent brain damage will occur, giving researchers a small timeframe to act.
- Seizures. Also, 10 minutes after the ischemia begins, some of the experimental animals may develop postischemic seizures which result in death.
- High mortality rate. Just after 15 minutes under this model, the impacts of this model become more evident and the majority of the animals will die.
- Requires surgery. Since the common carotid arteries are occluded, a surgical procedure will be necessary, in order to access them and anesthesia must be administered.
Cardiac Arrest and Resuscitation in Mice
The cardiac arrest model is typically carried out in larger animals, but special efforts have been made in order to create a modified model for mice.
In the cardiac arrest model for inducing global cerebral ischemia, the heart stops working temporarily, thus not delivering adequate blood to the brain. To cause cardiac arrest, mice are intravenously injected with KCl (potassium chloride). After 10 minutes while the mice are at a cardiac standstill, cardiopulmonary resuscitation (CPR) begins. The CPR routine is initiated with epinephrine administration, 100% oxygen ventilation, and chest compressions.
Advantages of the Cardiac Arrest Model
- Relevant to clinical reality. Since each year about 500,000 people have a cardiac arrest in the United States alone, there is clinical relevancy for using this model in order to identify new therapeutic interventions to improve outcome and recovery.
- Easy to induce. Since this model, in mice, only requires an injection of KCl and subsequent monitoring of body vitals. It is considered to be relatively simple when compared with the ischemic stroke models which require surgery.
Disadvantages of the Cardiac Arrest Model
- Relatively new model. This model was usually reserved for larger animals, such as dogs, and induced using electricity. Developing it for rodents is still something new and has only begun in the last few years. So, it may not be as well-validated as some of the other models are.
- Clinical complexity. Cardiac arrest is more complex than the ischemic model and many factors which might influence the outcome are not represented by this model.
Behavioral Outcomes of the Cardiac Arrest Model in Mice
One experiment set out to define the behavioral effects of the cardiac arrest model in mice. The C57BL/6 and 129SVEV models were used. The cardiac arrest model described above was applied. Mice were subjected to behavioral testing 24 hours before the model induction and then once more 3 or 7 days after they were resuscitated.
Both strains of post-ischemic mice had a reduced performance in the T-Maze as indicated by the reduced number of correct choices.
Temporary impairment was found in the Passive/Avoidance Task in both strains following resuscitation. The retention deficit was present on day 3 but not on day 7 for both strains, indicating that memory-related improvements were naturally occurring.
In the Open Field test, the C57BL/6 mouse strain was significantly more active as demonstrated by higher levels of locomotor activity. But, the researchers interpreted this as being due to strain differences and not necessarily ischemic-related.[65]
Furthermore, it was established that the cardiac arrest model is characterized by injuries to the caudoputamen and hippocampal regions of the mouse brain, lasting for at least a week after CPR.
Cerebral Venous Sinus Thrombosis Models
In contrast to global and focal cerebral ischemia which are localized to the blood vessels and arteries, venous thrombosis is a rare type of stroke caused by thrombosis in the dural venous sinuses. This cerebrovascular disorder has been noted to affect children and young adult more commonly than arterial stroke does and represented 0.5-3% of all stroke cases.[66]
Although cerebral veins and sinus thrombosis (CVT) has been induced in many different animals, rat models are considered to be amongst the most reliable due to the anatomy of their sinuses and brains.
Many methods exist that make CVT induction possible. The superior sagittal sinus can be occluded via direct injection of chemical substances. Commonly used chemicals to induce CVT are ethanolamine and cyanoacrylate. In general, sclerosing agents have been noted to be effective.
Another possibility is to use photochemical coagulation and rose bengal dye, (just as is done in photothrombotic models), on the dorsal cerebral veins in order to induce CVT in rats.[67] This model is known as the “two-vein occlusion model” (not to be confused with the two-vessel model) and is also used in clinical research.[68][69]
Other techniques which have been used for inducing CVT include subjecting the superior sagittal sinus to heat or mechanical damage. But, it has been established these two approaches (mechanical and heat-dependent means of occlusion) on their own do not successfully mimic the neuropathological consequences that occur in CVT and must be combined.
So, the best way to model CVT to date is by injecting thrombogenic cephalin suspension and then ligating superior sagittal sinus rostrally and caudally.[70] This way, the model reflects the thrombosis nature of the stroke and does not depend solely on mechanical or heat damage. Also, this method leads to lower mortality rates when compared to the collateral damage and mortality associated with injury or use of sclerosing agents.[71]
Advantages of CVT Models
- Opportunities for development. To date, there is no animal model available of spontaneously occurring CVT. Although this is a disadvantage, it is also an opportunity for further research.
- Used to study a rare disease. CVT models are a beginning for studying rare disease.
Disadvantages of CVT Models
- May require surgery. If the CVT model where ligatures and injection is chosen, then surgery is required for model induction. This brings a set of disadvantages to the table, including the chance of collateral damage due to operation.
- Do not reflect the complexity of CVT. The pathophysiology of CVT is not fully known yet. So, it is challenging to model accurately CVT given it’s not fully understood.
- No CVT-prone rodent strain exists. Since no go-to strain exists for this model, variation across experiments is bound to occur.
One of the main disadvantages of these models is the poor correlation between the neuropathological similarities in rat and human CVT episodes.[72]
In a clinical setting, advancements in technology have made improved diagnosis and prognosis possible,[73] but more research needs to be done in order to improve the existing animal models.
Different Mouse Strains Affect Ischemic Stroke Modeling
Although using mice for research is cost and time effective, there are some things to consider when working with them. Mouse strains are known to affect ischemic stroke modeling outcomes due to inter-strain differences and varying ischemic sensitivities.
So, while using mice with a similar genetic background increases the reproducibility of the experiment, there are some inter-strain variables that may affect results, especially in instances for developing therapeutic agents for ischemic strokes. Below are three major areas (vascular anatomy, blood flow, and inflammatory response) which vary across mouse strains and, thus, will affect ischemic stroke modeling.
Mouse Strain Differences in Cerebral Vascular Anatomy
In an experiment studying how three different mouse strains (BALB/C, CFW, and BDF strains) are affected by focal ischemia, it was found that the three strains have significant differences in their susceptibility to ischemic stroke.[74]
During MCAo, the infarct volume averages (in mm3) were reported to be 23 in BALB/C mice, 15 in CFW mice, and 5 in BDF mice.
In a different condition, MCAo was combined with ipsilateral common carotid artery occlusion (CCAO). This led to infarct volumes that were 72 in BALB/C mice, 38 in CFW mice, and 15 in BDF mice. The mortality rate of this procedure was 67% in BALB/C mice and 42% in CFW and nothing in BDF mice. Such figures demonstrate large strain differences and responses to ischemic stroke modeling.
When subjected only to CCAO, only the BALB/C mice had hemispheric infarctions (in 36% of all BALB/C mice) and the other two strains did not.
Physiological variables (arterial blood pressures, blood cell profiles, and blood gases) remained similar across all three mouse strains. But, carbon black studies revealed differences in anatomical data.
Comparing BALB/C with BDF mice, BALB/C mice had a decrease in the frequency which the parent posterior communicating arteries were joined, meaning their anatomical structure is such that their Circle of Willis will be incomplete most of the time. Compared with CFW mice, the BALB/C mice showed incompletion of their vascular anatomy only some of the time.[74]
These findings, demonstrating vascular variations and infarct size differences based on the method of occlusion, show that different strains have different susceptibilities to modeling ischemic stroke.
Differences in Cerebral Blood Flow Based on Mouse Strain
Blood flow also varies by mouse strain. For example, BALB/C mice have less cerebral arterial branches than C57BL/6 mice do. Based on differences in vascular structure, cerebral blood flow differences will follow.
In an experiment comparing these two mouse strains in terms of the middle cerebral artery’s blood flow dynamics, it was established that there are significant differences.
The researchers used noninvasive optical imaging, more specifically indocyanine green (ICG) imaging. The C57BLB/C had lower relative maximum fluorescence intensity (Imax) values and also the time that ICG needed to reach the Imax was lower in the C57BLB/C mice compared to the BALB/C mice.
The researchers interpreted these findings to mean that the C57BLB/C mice yield lower blood flow per cerebral artery due to their higher number of arterial branches.[75]
Comparison of Inflammatory Response in C57BL/6 and FVB Mice
Inflammatory response is another factor that varies with mouse strain. Inflammatory cells and their response are of interest to researchers because they possibly contribute to the secondary brain injury which follows after the primary injury from the ischemic stroke has occurred.
One experiment studied the immune responses in C57BL/6 and FVB mice after MCAo and established that there were significant differences in immune responses between the two mice.
The mice were subjected to 1 hour of MCAo followed by 23 hours of reperfusion. The infarct size was equal in the two strains, but functional deficits and inflammatory responses were not.
The C57BL/6 mice had a greater number of CD45+ leukocytes in their brains after the ischemic episode. Furthermore, the C57BL/6 mice had mostly T and B lymphocytes in their inflammatory response. The FVB mice, on the other hand, had mostly monocytes, macrophages, and neutrophils making up their inflammatory response.[76]
Functionally, the C57BL/6 mice displayed greater deficits in the hanging wire test and had lower scores in the neurological scoring test than the FVB mice did.
The researchers interpreted these findings as supportive of the concept that post-stroke functional outcome depends on the composition of immune cells which develop in response to the brain ischemia.
Most Commonly Used Rodent Strains in Ischemic Stroke Research
Some mice or rat strains are more commonly used than others for modeling ischemic stroke. Since strain can affect many outcomes, such as the infarct size, it is an important factor which researchers must consider prior to beginning their experiment.
Some of the commonly used mice and rodent strains are:[51]
- Spontaneously hypertensive rats. These rats offer large infarct and low variation in their size. Plus, are useful for modeling obesity and hypertension, two risk factors of ischemic stroke.
- Sprague-Dawley rats. Sprague-Dawley rats have small infarct volumes combined with high variability. It is estimated that about 60% of all preclinical stroke research with neuroprotection data utilized Sprague-Dawley rats.
- Wistar rats. Wistar rats are thought to have the lowest variability in the infarct size they produce.
- C57BL/6 mice. Under permanent MCAo conditions, these mice produce larger infarct volumes than Sv129 mice. Also, out of many mouse strains, C57BL/6 is considered to be the most susceptible to ischemia after a bilateral common carotid occlusion.[77]
Therefore, the strain that is selected plays an important role in determining the quality and characteristics of the ischemia that will form.
Overview of Assessment Methods of Ischemic Brain Injury
In this section, we will discuss how researchers assess ischemic brain injury in rodent models, in order to determine how stroke impacts the brain and its processes.
Bioluminescence Methods in Ischemic Stroke Research
The most commonly studied substrates using pictorial bioluminescence methods are glucose, ATP, and lactate. A substrate and its enzymes are paired with a light emitting system. Then, cryostat sections are combined with a frozen reaction mix until diffusion occurs. There is a correlation between the light emitted and the substrate’s concentration levels. The light emitted is recorded through a specific camera or with photographic film.
In ischemic stroke research, pictorial bioluminescence methods measuring ATP are applied in order to identify the stroke’s ischemic core. Since there is a relationship between energy metabolism (needing ATP) and blood flow, this method precisely identifies which areas are depleted in ATP.[47]
Fluorescence Methods
In brain ischemia, when the tissue’s pH balance undergoes acidosis and anaerobic glucose utilization is occurring, brain images can be acquired and assessed. The tissue’s pH is imaged fluoroscopically. A brain section is placed on top of a filter paper which is soaked in umbelliferone (a fluorescent pH indicator). Then at 340 and 370 nm excitation, the difference in fluorescence creates an image to be recorded.
NADH Fluorescence Imaging
NADH fluorescence is also used to capture ischemia because it shows the redox state of the sampled brain tissue. Excitation at 450 nm is used to acquire NADH images.
Mapping of Gene Expression in Ischemic Stroke Research
Using cryostat sections, gene expression can be evaluated at the transcriptional and translational stages. This is achieved by using cDNA in situ hybridization together with immunochemistry.
In ischemic research, the stress genes HO-1 and hsp70 are usually of interest because they are related to the stroke’s penumbra.
Other genes that are studied using this assessment method are the c-jun, junB, and c-fos genes. These immediate early genes become active when there are peri-infarct depression waves spreading across the brain parenchyma. These genes can be found in the penumbra and also in the ipsilateral hemisphere.
Multi-tracer Autoradiography
Multi-pixel threshold analysis is achieved through this method. Multitracer autoradiography is applied in junction with bioluminescence methods and can be used to quantify the pictorial measurements of glucose utilization, blood flow, and protein synthesis. In the triple tracer autoradiographic technique, glucose utilization, blood flow, and protein synthesis are all measured together by means of quantifying the 3H-labeled amino acids.[78] It is important to identify and quantify such cellular process given that they are crucial for homeostasis.
Behavioral Methods
Behavioral methods are an important step in ischemic stroke research. Since a lot of stroke research is dedicated towards rehabilitating behaviors debilitated by stroke, behavioral methods in animals are a large area of focus for scientists. The following behavioral tests are commonly used in stroke research using animals in order to assess a variety of abilities, from physical to cognitive functioning:
Cylinder Test
When a rodent is placed inside a transparent cylinder, it will naturally put its forelimbs on the sides (walls) of the cylindrical chamber and try to move upwards (a behavior known as rearing). In instances of ischemic stroke, a rodent is likely to have contralateral or ipsilateral immobility in its forelimbs. Therefore, the Cylinder Test is used to quantify a rodent’s spontaneous use of forelimbs and is relevant to ischemic stroke research.
Grid Walking
Grid walking, also known as the Horizontal Grid Test, is a behavioral test wherein the mouse is placed on an elevated mesh grid and its balance, coordination, and precision in paw placement are measured. Motor coordination is one of the most common disabilities observed in ischemic stroke patients. Thus, grid walking is a commonly used assessment of ischemic stroke behavioral studies.
Horizontal Ladder
In the Horizontal Ladder Test, also referred to as the Ladder Rung Walking test, fore- and hindlimb functionality is assessed based on subsequent placing, stepping, and inter-limb coordination. A ladder is placed flat and rodent is closed off so it is directed to move across the ladder rungs. This test is combined with video analysis, in order to get an accurate measure of foot faults and limb movement.
Ledged Tapered Beam
Since the cylinder test is used to assess forelimbs, there is also a test used to assess the level of hindlimb functioning in rodents: the Ledged Tapered Beam, or the ‘Balance Beam,’ for short. In this test, front paw slips are considered to be rare, so analysis focuses on hindlimb slips. If the ischemic stroke affects the motor area regions of the brain, hindlimb functionality is bound to be compromised. Therefore, many tests are usually used in ischemic stroke behavioral studies, in order to analyze fully a rodent’s motor abilities and detect any improvements due to intervention.
Skilled Forelimb Test
The Skilled Forelimb Test, also referred to as Reaching Chamber/Pellet Retrieval, assesses an animal’s ability to reach for a food pellet that is located within reaching distance. The rodent is placed in a chamber containing a small opening where only its paw can pass through. So, a pellet is placed outside of the chamber, but close enough for the rodent to reach it. Typically, the pellet is placed contralaterally to the reaching limb for the purpose of evaluating any possible unilateral brain impairments due to stroke. Impairments are determined by quantifying successes, attempts, drops, and failures to retract the pellet.
The Corner Test
This test is a simple, reliable method for identifying postural asymmetries and sensorimotor deficits in rodents that have been used to model ischemic stroke. Essentially, a rodent is placed in the corner, formed by two boards coming together at a 30-degree angle. When its vibrissae are stimulated, the rodent will immediately rear and turn. Healthy rodents are equally likely to turn right or left while those with unilateral brain damage are more biased towards the ipsilateral side.[21]
Adhesive Removal Test
This test is used for determining any impairments of tactile sensation due to stroke. To run this test, two adhesive tapes which are equally sized are placed under the animal’s paws from which animals are expected to remove simply by grooming. Rodents with unilateral brain damage from ischemic stroke are biased in removing first the adhesive from the ipsilateral limb.
Rotarod
Using the Rotarod, a device which rotates at an accelerating speed, a rodent’s balance, and motor coordination are quantified. Mice and rats that have suffered from brain ischemia are able to stay a significantly shorter amount of time on the Rotarod when compared to healthy controls.[79]
The Staircase Test
The Staircase Test, also known as the Stairway Test, can be used to evaluate sensorimotor-related deficits in rodents that have suffered from stroke. This test is similar to the Rotarod, Tilt Ladder, Balance Beam, and Horizontal Ladder. It was developed by Boltze et al. specifically for the purpose of testing sensorimotor function in rats that had middle cerebral artery occlusion.[80] Using a mounted ladder that is triangularly shaped, rodents are placed about 20cm from the ladder’s apex and are expected to climb upwards, in order to reach their home cage. Rodents with impairments from stroke do not take a direct path and are highly likely to deviate. Also, using this test, forelimb extension, side bias, and grasping skills are all measured.
Composite Scores
A variety of tests are administered (sensory, reflex, balance, and motor) and the scores of each test are tallied up into a composite score.
Morris Water Maze
The Morris Water Maze is a cognitive assessment tool which measures spatial learning abilities. A rodent is placed in an opaque pool of water and is expected to find an escape platform and remember it through continuous training. Animals modeling ischemic stroke damage have compromised performance in this task. Therefore, it can be a very useful cognitive measure when assessing stroke-related interventions relating to memory functions.
Radial Arm Maze
The Radial Arm Maze is another cognitive tool for measuring memory. Researchers use it when they specifically want to focus on working and reference memory. A mouse is placed in a maze which contains 8 or 12 different arms, all projecting from the center, and has food targets located at the end of the arms. Therefore, mice are expected to learn the location of food rewards. Studies on rodents which had an ischemic stroke reveal mixed findings as to how reference and working memory are affected by ischemic stroke in rats and mice.
Non-Invasive Multimodal Imaging
Non-invasive multimodal imaging is a heavily used method for assessing ischemic stroke. The two most common non-invasive imaging methods for capturing ischemic stroke are positron-emission tomography (PET) and magnetic resonance imaging (MRI).
Positron-Emission Tomography in Ischemic Stroke Research
PET can be used for measuring glucose and oxygen consumption in brain ischemia as well as blood flow and the oxygen extraction fraction, a measurement used to reliably identify the penumbra and irreversibly damaged brain tissue. PET is also used to image certain ligands, such as flumazenil, and whether they bind to their receptors.
How PET is Used to Detect the Ischemic Core
Ischemic stroke is characterized by an increased blood oxygen extraction fraction due to the decreasing blood flow. This happens in order to fulfill the oxygen requirements needed in aerobic metabolic processes. When the flow value drops to 50% of that of the control’s, the brain tissue is said to become hypoxic. When the tissue is hypoxic, anaerobic glycolysis predominates because oxygen consumption is low. However, when the flow continues to decrease, anaerobic glycolysis will also start to fail. At this point, energy metabolism stops, the brain tissue is said to have necrotized, and 11C-flumazenil and other ligands will no longer be capable of binding to their receptors. The decrease in ligand binding and/or the reduction of glucose and oxygen consumption describes the ischemic core.
The penumbra is characterized by an increase of the oxygen extraction fraction or an increase in glucose utilization. The penumbra is also imaged by means of hypoxia markers like 18F-nitroimidazole (F-MISO). F-MISO is trapped in hypoxic tissue, not in necrotic or normoxic brain tissue. So, it is specific to the penumbra.
It should be noted that PET is less reliable than histological sections due to its high scatter of tracer concentrations and low spatial resolution, but it is still commonly used in research.
In summary, the ischemic area is defined by a decline in cerebral blood flow while the penumbra is defined by an increase in the oxygen extraction fraction. The core is demarcated by the suppression of glucose utilization and the cerebral metabolic rate of oxygen.
Magnetic Resonance Imaging
MRI is used in ischemic stroke research in order to capture structural differences which result due to stroke. Recent technological developments and advanced techniques, which will be discussed below, have made it possible to use MRI scanners in such a way that a variety of information gets captured.
MRI Techniques Applied in Preclinical Stroke Research
Magnetic Resonance Angiography
Magnetic resonance angiography (MRA) is used in order to visualize the occlusion status of a specified blood vessel which was targeted during model induction. In contrast to traditional angiography which uses an inserted tube in order to image blood vessels, MRA is non-invasive.[81]
Perfusion-Weighted Imaging
Perfusion-weighted imaging (PWI) is an MRI technique used in ischemic stroke research to make serial cerebral blood flow maps which depict the location and severity of the ischemic injury. PWI also shows if any induced or spontaneous reperfusion has occurred and any possible drug-induced alterations in cerebral blood flow.
Diffusion-Weighted Imaging
Diffusion-weighted imaging (DWI) is used with the apparent diffusion coefficient (ADC) of water to create serial maps which display brain swelling and any acute or evolving brain injury. A decreased ADC together with an increase in the DWI signal means that occlusion has taken place and that injured brain tissue exists. Therefore, this method allows for the identification of ischemia within minutes. Such a quick time frame is an advantage because hours may need to pass before an infarct can be identified through MRI and other more traditional approaches.
Also, DWI can be used to study therapeutic effects in ischemic stroke research, particularly in thrombosis animal models.[82]
PWI/DWI Mismatch
Combining DWI with PWI has led to the development of the PWI/DWI mismatch concept. This concept states that the penumbra of a stroke is defined by the area that has reduced blood flow but which DWI or ADC changes are absent. Although this is a commonly used technique in literature, it has received some points of resistance and debate. Therefore, consideration should be taken and additional research should be done to further develop this technique.
Diffusion Tensor Imaging
Diffusion tensor imaging (DTI) is a way of visualizing the brain’s white matter tracts. Specific MRI settings combined with software enable scientists to get a closer look at the brain’s white matter. This is useful for ischemic stroke research which focuses on how stroke impacts the brain’s structure.
Functional MRI and Stimulation
Functional MRI (fMRI) is a technique which is applied in order to asses function or loss of function in an ischemic brain region. Brain activity is measured with fMRI by detecting changes in regional blood flow associated with increased brain activity. This technique is based on the assumption that neuronal activity is coupled with cerebral blood flow.
In ischemic stroke research, serial fMRI studies can reveal how the damaged brain regions respond to stimulation, establish brain activity, and help identify whether any compensatory changes have occurred in response to the injury.
Enhanced Contrast T1-Weighted Imaging
When MRI scans are manipulated in order to enhance the contrast of the image, a breakdown in the blood-brain barrier may be identified.
By being able to image the blood-brain barrier, it is possible to develop accurate animal models and study how therapeutic developments, such as pharmacological or neuroprotective compounds, may affect the brain.
The Major Human Arteries and Post-Stroke Clinical Symptoms
One of the challenges of modeling ischemic stroke in rodents deals with aligning the location of the stroke with the subsequent neurological deficits. Below is a brief review of clinical symptoms and changes in behaviors and cognition in humans which are associated with ischemic stroke in specific arteries.[83]
Anterior Cerebral Artery
Ischemic stroke to the anterior cerebral artery is associated with: contralateral sensory losses, contralateral psychomotor disorders, homolateral ataxia in the arm, mental manifestations, and behavioral alterations.
Basilar Artery
When an ischemic stroke occurs in the basilar artery the clinical symptoms that appear are speech impairment, transient ischemic attacks (“mini-strokes” lasting for a short time, no more than 5 minutes), sensitivity, facial paralysis, dysarthria, and contralateral hemiplegia.
Internal Carotid Artery
If the internal carotid artery is the location for the ischemic stroke, the following clinical symptoms may arise retinal ischemia with blindness or numbness in the ipsilateral eye, thrombosis, recurrent transient attacks, and contralateral hemiplegia with aphasia.
Middle Cerebral Artery
An ischemic stroke in the middle cerebral artery is also associated with serious motor and cognitive problems, including apraxia, aphasia, and contralateral hemiparesis and/or hemiplegia.
MCAo models and experiments already discussed in this article have demonstrated the deficits associated with a blockage in this artery in mice and rats.
Posterior Cerebral Artery
The clinical symptoms linked to an ischemic stroke in the posterior cerebral artery are ataxia, dyslexia without agraphia, memory disorders, and thalamic sensory syndrome.
Since ischemic stroke in certain areas is correlated with specific symptoms, more efforts are needed in order to develop and advance models so that they can translate more accurately to human subjects.
Treatment Options for Ischemic Stroke
Animal models of ischemic stroke can be used to study treatment options, in order to develop and advance healthcare. Yet, even though research on ischemic stroke spans the course of decades, treatment options are still severely limited.[84] Currently, the only drug which has been approved for ischemic stroke treatment, as mentioned previously, is rtPA, and even this drug possesses the risk of creating hemorrhages. Therefore, only a small amount of patients will be subjected to treatment with rtPA.
A further issue of concern is that there are no existing treatments approved for targeting the pathological responses which occur after the brain ischemia has resulted, such as oxidative stress, apoptosis, or inflammation.
Future Directions for Developing Animal Models for Stroke Therapy
Future directions for using animal models in ischemic stroke research should focus on how to use these models in order to model therapy and recovery accurately. It is important to develop models which reflect human pathophysiology, in order to increase translatability across findings and application.
A current problem in clinical trials and animal models is that they only focus on the stroke size without localizing the stroke to particular circuits in the brain. For example, many animal model studies have been criticized for only being focused on decreasing the stroke size. The post-stroke deficits in humans occur due to damage in a certain area of the brain, such as the motor cortex. So, future interventions and models using rodents need to reflect these issues and focus on how to utilize functional remapping and reorganization from the spared circuits in order to target those damaged by the infarct.[5]
Modeling Comorbidities
In addition to developing models, more research is needed in order to establish how certain comorbidities affect animal model research and subsequent behavioral and cognitive outcomes. Comorbidities are
diseases which occur simultaneously with each other. Common comorbidities for ischemic stroke include diabetes, hypertension, and coronary disease.
Although spontaneous stroke models with their use of certain strains do reflect the issue of comorbidity, most models do not take such precautions in capturing ischemic stroke. More research is needed to show how outcomes relating to ischemic stroke change by using mice with these comorbidities.
Future Research
Ischemic animal model researchers have plenty of models to pick from. But, one of the major challenges and disadvantages of these models is that they do not translate perfectly to human ischemic stroke.
Based on the models discussed in this article, ideas and research questions can be made for the purpose of expanding the knowledge available on ischemic stroke.
References
- Stam, Jan. “Thrombosis of the cerebral veins and sinuses.” New England Journal of Medicine 352.17 (2005): 1791-1798.
- Park, Hyun-Young, et al. “Multifocal strokes as the initial manifestation of metastatic tumors.” The neurologist 16.5 (2010): 322-324.
- Traystman, Richard J. “Animal models of focal and global cerebral ischemia.” ILAR journal 44.2 (2003): 85-95.
- Sun, Ming-Shuo, et al. “Free Radical Damage in Ischemia-Reperfusion Injury: An Obstacle in Acute Ischemic Stroke after Revascularization Therapy.” Oxidative medicine and cellular longevity 2018 (2018).
- Carmichael, S. Thomas. “Rodent models of focal stroke: size, mechanism, and purpose.” NeuroRx 2.3 (2005): 396-409.
- Kassem-Moussa, Hassan, and Carmelo Graffagnino. “Nonocclusion and spontaneous recanalization rates in acute ischemic stroke: a review of cerebral angiography studies.” Archives of neurology 59.12 (2002): 1870-1873.
- Ren, Changhong, et al. “Animal Stroke Model: Ischemia–Reperfusion and Intracerebral Hemorrhage.” Injury Models of the Central Nervous System. Humana Press, New York, NY, 2016. 373-390.
- Tamura, A_, et al. “Focal cerebral ischaemia in the rat: 1. Description of technique and early neuropathological consequences following middle cerebral artery occlusion.” Journal of Cerebral Blood Flow & Metabolism 1.1 (1981): 53-60.
- Tamura, Akira, et al. “Protection from cerebral ischemia by a new imidazole derivative (Y-9179) and pentobarbital. A comparative study in chronic middle cerebral artery occlusion in cats.” Stroke 10.2 (1979): 126-134.
- Herson, Paco S., and Richard J. Traystman. “Animal models of stroke: translational potential at present and in 2050.” Future neurology 9.5 (2014): 541-551.
- Markgraf, Carrie G., et al. “Comparative histopathologic consequences of photothrombotic occlusion of the distal middle cerebral artery in Sprague-Dawley and Wistar rats.” Stroke 24.2 (1993): 286-292.
- Durukan, Aysan, and Turgut Tatlisumak. “Acute ischemic stroke: overview of major experimental rodent models, pathophysiology, and therapy of focal cerebral ischemia.” Pharmacology Biochemistry and Behavior 87.1 (2007): 179-197.
- Howells, David W., et al. “Different strokes for different folks: the rich diversity of animal models of focal cerebral ischemia.” Journal of Cerebral Blood Flow & Metabolism 30.8 (2010): 1412-1431.
- Schmid-Elsaesser, Robert, et al. “A critical reevaluation of the intraluminal thread model of focal cerebral ischemia: evidence of inadvertent premature reperfusion and subarachnoid hemorrhage in rats by laser-Doppler flowmetry.” Stroke 29.10 (1998): 2162-2170.
- Dittmar, Michael, et al. “External carotid artery territory ischemia impairs outcome in the endovascular filament model of middle cerebral artery occlusion in rats.” Stroke 34.9 (2003): 2252-2257.
- Liu, Shimin, et al. “Rodent stroke model guidelines for preclinical stroke trials.” Journal of experimental stroke & translational medicine 2.2 (2009): 2.
- Garcia, Julio H., Kai-Feng Liu, and Khang-Loon Ho. “Neuronal necrosis after middle cerebral artery occlusion in Wistar rats progresses at different time intervals in the caudoputamen and the cortex.” Stroke 26.4 (1995): 636-643.
- Kilic, Ertugrul, et al. “Delayed melatonin administration promotes neuronal survival, neurogenesis and motor recovery, and attenuates hyperactivity and anxiety after mild focal cerebral ischemia in mice.” Journal of pineal research 45.2 (2008): 142-148.
- Al-Qazzaz, Noor Kamal, et al. “Cognitive impairment and memory dysfunction after a stroke diagnosis: a post-stroke memory assessment.” Neuropsychiatric disease and treatment 10 (2014): 1677.
- Markgraf, Carrie G., et al. “Sensorimotor and cognitive consequences of middle cerebral artery occlusion in rats.” Brain research 575.2 (1992): 238-246.
- Schaar, Krystal L., Miranda M. Brenneman, and Sean I. Savitz. “Functional assessments in the rodent stroke model.” Experimental & translational stroke medicine 2.1 (2010): 13.
- Sommer, Clemens J. “Ischemic stroke: experimental models and reality.” Acta neuropathologica 133.2 (2017): 245-261.
- Barber, Philip A., et al. “Temperature-regulated model of focal ischemia in the mouse: a study with histopathological and behavioral outcomes.” Stroke 35.7 (2004): 1720-1725.
- Tamura, A_, et al. “Focal cerebral ischaemia in the rat: 1. Description of technique and early neuropathological consequences following middle cerebral artery occlusion.” Journal of Cerebral Blood Flow & Metabolism 1.1 (1981): 53-60.
- Buchan, Alastair M., Dong Xue, and Andrew Slivka. “A new model of temporary focal neocortical ischemia in the rat.” Stroke 23.2 (1992): 273-279.
- Yanamoto, Hiroji, et al. “Evaluation of MCAO stroke models in normotensive rats: standardized neocortical infarction by the 3VO technique.” Experimental neurology 182.2 (2003): 261-274.
- Kleinschnitz, Christoph, et al. “Blocking of platelets or intrinsic coagulation pathway–driven thrombosis does not prevent cerebral infarctions induced by photothrombosis.” Stroke 39.4 (2008): 1262-1268.
- Watson, Brant D., et al. “Induction of reproducible brain infarction by photochemically initiated thrombosis.” Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society 17.5 (1985): 497-504.
- Hilger, Thomas, et al. “Characterization of a novel chronic photothrombotic ring stroke model in rats by magnetic resonance imaging, biochemical imaging, and histology.” Journal of Cerebral Blood Flow & Metabolism 24.7 (2004): 789-797.
- Hu, XiaoLei, et al. “Progressive and reproducible focal cortical ischemia with or without late spontaneous reperfusion generated by a ring-shaped, laser-driven photothrombotic lesion in rats.” Brain Research Protocols 7.1 (2001): 76-85.
- Lee, Vee Meng, et al. “Evolution of photochemically induced focal cerebral ischemia in the rat: magnetic resonance imaging and histology.” Stroke 27.11 (1996): 2110-2119.
- Kim, Hyung-Sun, et al. “A rat model of photothrombotic capsular infarct with a marked motor deficit: a behavioral, histologic, and microPET study.” Journal of Cerebral Blood Flow & Metabolism 34.4 (2014): 683-689.
- Kuroiwa, Toshihiko, et al. “Development of a rat model of photothrombotic ischemia and infarction within the caudoputamen.” Stroke 40.1 (2009): 248-253.
- Lu, Hongyang, et al. “Induction and imaging of photothrombotic stroke in conscious and freely moving rats.” Journal of Biomedical Optics 19.9 (2014): 096013.
- Yu, Cheng-Long, et al. “Whole-scale neurobehavioral assessments of photothrombotic ischemia in freely moving mice.” Journal of neuroscience methods 239 (2015): 100-107.
- Robinson, M. J., et al. “Reduction of local cerebral blood flow to pathological levels by endothelin-1 applied to the middle cerebral artery in the rat.” Neuroscience letters 118.2 (1990): 269-272.
- Hughes, P. M., et al. “Focal lesions in the rat central nervous system induced by endothelin-1.” Journal of Neuropathology & Experimental Neurology 62.12 (2003): 1276-1286.
- Endothelin-1 induced lesions of the frontoparietal cortex of the rat. A possible model of focal cortical ischemia.
- Bogaert, L., et al. “Neurochemical changes and laser Doppler flowmetry in the endothelin-1 rat model for focal cerebral ischemia.” Brain research 887.2 (2000): 266-275.
- Frost, Shawn B., et al. “An animal model of capsular infarct: endothelin-1 injections in the rat.” Behavioural brain research 169.2 (2006): 206-211.
- Ward, Nick M., et al. “Simple and choice reaction-time performance following occlusion of the anterior cerebral arteries in the rat.” Experimental brain research 123.3 (1998): 269-281.
- Tennant, Kelly A., and Theresa A. Jones. “Sensorimotor behavioral effects of endothelin-1 induced small cortical infarcts in C57BL/6 mice.” Journal of neuroscience methods 181.1 (2009): 18-26.
- Sommer, Clemens J. “Ischemic stroke: experimental models and reality.” Acta neuropathologica 133.2 (2017): 245-261.
- Wang, Chen Xu, et al. “Patency of cerebral microvessels after focal embolic stroke in the rat.” Journal of Cerebral Blood Flow & Metabolism 21.4 (2001): 413-421.
- Ren, Ming, et al. “Embolic middle cerebral artery occlusion model using thrombin and fibrinogen composed clots in rat.” Journal of neuroscience methods 211.2 (2012): 296-304.
- Lam, Carson K., et al. “Embolus extravasation is an alternative mechanism for cerebral microvascular recanalization.” Nature 465.7297 (2010): 478.
- Hossmann, Konstantin-Alexander. “Cerebral ischemia: models, methods and outcomes.” Neuropharmacology 55.3 (2008): 257-270.
- Kudo, M., et al. “An animal model of cerebral infarction. Homologous blood clot emboli in rats.” Stroke 13.4 (1982): 505-508.
- Beech, John S., et al. “Further characterisation of a thromboembolic model of stroke in the rat.” Brain research 895.1-2 (2001): 18-24.
- Orset, Cyrille, et al. “Mouse model of in situ thromboembolic stroke and reperfusion.” Stroke 38.10 (2007): 2771-2778.
- Fluri, Felix, Michael K. Schuhmann, and Christoph Kleinschnitz. “Animal models of ischemic stroke and their application in clinical research.” Drug design, development and therapy 9 (2015): 3445.
- Fukuchi, Kazuki, et al. “Correlation of sequential MR images of microsphere-induced cerebral ischemia with histologic changes in rats.” Investigative radiology 34.11 (1999): 698.
- Mayzel-Oreg, Orna, et al. “Microsphere-induced embolic stroke: An MRI study.” Magnetic Resonance in Medicine: An Official Journal of the International Society for Magnetic Resonance in Medicine 51.6 (2004): 1232-1238.
- Rapp, Joseph H., et al. “Microemboli composed of cholesterol crystals disrupt the blood-brain barrier and reduce cognition.” Stroke 39.8 (2008): 2354-2361.
- Gerriets, Tibo, et al. “The macrosphere model: evaluation of a new stroke model for permanent middle cerebral artery occlusion in rats.” Journal of neuroscience methods 122.2 (2003): 201-211.
- Okakomoto Aoki, K. “Development of a strain of spontaneously hypertensive rat.” Japanese Circulation Journal 27 (1963): 282-293.
- Bailey, Emma L., et al. “Is the spontaneously hypertensive stroke prone rat a pertinent model of sub cortical ischemic stroke? A systematic review.” International Journal of Stroke 6.5 (2011): 434-444.
- Bailey, Emma L., et al. “Potential animal models of lacunar stroke: a systematic review.” Stroke 40.6 (2009): e451-e458.
- Hainsworth, Atticus H., and Hugh S. Markus. “Do in vivo experimental models reflect human cerebral small vessel disease? A systematic review.” Journal of Cerebral Blood Flow & Metabolism 28.12 (2008): 1877-1891.
- Deng, Ping, and Zao C. Xu. “Four-vessel occlusion model in rats.” Animal Models of Acute Neurological Injuries. Humana Press, 2009. 65-76.
- Pulsinelli, William A., and JAMES B. Brierley. “A new model of bilateral hemispheric ischemia in the unanesthetized rat.” Stroke 10.3 (1979): 267-272.
- O’Neill, Michael J., and James A. Clemens. “Rodent models of focal cerebral ischemia.” Current protocols in neuroscience 12.1 (2000): 9-6.
- Raval, Ami P., Chunli Liu, and Bingren R. Hu. “Rat Model of Global Cerebral Ischemia: The Two-Vessel Occlusion (2VO) Model of Forebrain Ischemia.” Animal Models of Acute Neurological Injuries. Humana Press, 2009. 77-86.
- Smith, Maj‐Lis, et al. “Models for studying long‐term recovery following forebrain ischemia in the rat. 2. A 2‐vessel occlusion model.” Acta neurologica Scandinavica 69.6 (1984): 385-401.
- Kofler, Julia, et al. “Histopathological and behavioral characterization of a novel model of cardiac arrest and cardiopulmonary resuscitation in mice.” Journal of neuroscience methods 136.1 (2004): 33-44.
- Yenigün, Mesut, et al. “Sinus thrombosis—do animal models really cover the clinical syndrome?.” Annals of translational medicine 3.10 (2015).
- Nakase, Hiroyuki, et al. “Use of Local Cerebral Blood Flow Monitoring to Predict Brain Damage after Disturbance to the Venous CirculationCortical Vein Occlusion Model by Photochemical Dye.” Neurosurgery 37.2 (1995): 280-286.
- Kimura, R., et al. “Vascular endothelial growth factor antagonist reduces brain edema formation and venous infarction.” Stroke 36.6 (2005): 1259-1263.
- Nakagawa, Ichiro, et al. “MitoKATP-channel opener protects against neuronal death in rat venous ischemia.” Neurosurgery 57.2 (2005): 334-340.
- Röther, Joachim, et al. “Experimental cerebral venous thrombosis: evaluation using magnetic resonance imaging.” Journal of Cerebral Blood Flow & Metabolism 16.6 (1996): 1353-1361.
- Frerichs, Kai U., et al. “Cerebral sinus and venous thrombosis in rats induces long-term deficits in brain function and morphology—evidence for a cytotoxic genesis.” Journal of Cerebral Blood Flow & Metabolism 14.2 (1994): 289-300.
- Durukan, Aysan, and Turgut Tatlisumak. “Acute ischemic stroke: overview of major experimental rodent models, pathophysiology, and therapy of focal cerebral ischemia.” Pharmacology Biochemistry and Behavior 87.1 (2007): 179-197.
- Stam, Jan. “Thrombosis of the cerebral veins and sinuses.” New England Journal of Medicine 352.17 (2005): 1791-1798.
- Barone, F. C., et al. “Mouse strain differences in susceptibility to cerebral ischemia are related to cerebral vascular anatomy.” Journal of Cerebral Blood Flow & Metabolism 13.4 (1993): 683-692.
- Kang, Hye-Min, et al. “Optical measurement of mouse strain differences in cerebral blood flow using indocyanine green.” Journal of Cerebral Blood Flow & Metabolism 35.6 (2015): 912-916.
- Kim, Hyun Ah, et al. “Brain immune cell composition and functional outcome after cerebral ischemia: comparison of two mouse strains.” Frontiers in cellular neuroscience 8 (2014): 365.
- Yang, Gongming, et al. “C57BL/6 strain is most susceptible to cerebral ischemia following bilateral common carotid occlusion among seven mouse strains: selective neuronal death in the murine transient forebrain ischemia.” Brain research 752.1-2 (1997): 209-218.
- Mies, Günter. “Multi-Tracer Autoradiography for the Simultaneous Measurement of Cerebral Blood Flow and Metabolism.” Cerebral Blood Flow. Springer, Boston, MA, 1988. 67-90.
- Bouët, Valentine, et al. “Sensorimotor and cognitive deficits after transient middle cerebral artery occlusion in the mouse.” Experimental neurology 203.2 (2007): 555-567.
- Boltze, Johannes, et al. “The stairway: a novel behavioral test detecting sensomotoric stroke deficits in rats.” Artificial organs 30.10 (2006): 756-763.
- Macrae, I. M. “Preclinical stroke research–advantages and disadvantages of the most common rodent models of focal ischaemia.” British journal of pharmacology 164.4 (2011): 1062-1078.
- Langhauser, Friederike L., et al. “Thromboembolic stroke in C57BL/6 mice monitored by 9.4 T MRI using a 1H cryo probe.” Experimental & translational stroke medicine 4.1 (2012): 18.
- Casals, Juliana B., et al. “The use of animal models for stroke research: a review.” Comparative medicine 61.4 (2011): 305-313.4
- Majid, Arshad. “Neuroprotection in stroke: past, present, and future.” ISRN neurology 2014 (2014).