A myocardial infarction (MI), commonly known as a heart attack, is a medical incident where muscle tissue in the heart is damaged by lack of blood flow. Pain in the chest and upper body, trouble breathing, exhaustion and nausea are the most common signs, although an MI can be entirely symptomless. If a significant portion of the heart’s muscle tissue is destroyed, MI can lead to congestive heart failure (CHF), a condition where the heart is no longer able to pump enough blood to provide oxygen to all the body’s organs and tissues.
Over 600,000 people in the US suffer an MI each year,[1] and around 2% of the US population is suffering from CHF. Over half of these individuals die within 15 years of first contracting the disease.[2] The severe prevalence and mortality rate of MI and CHF, combined with increased risk factors for these diseases in the population, makes scientific research into their pathology extremely important. In place of human patients, mouse models are often used for such research. Using mice incurs fewer ethical concerns, and being mammals their brain and behavior are relatively similar to humans.
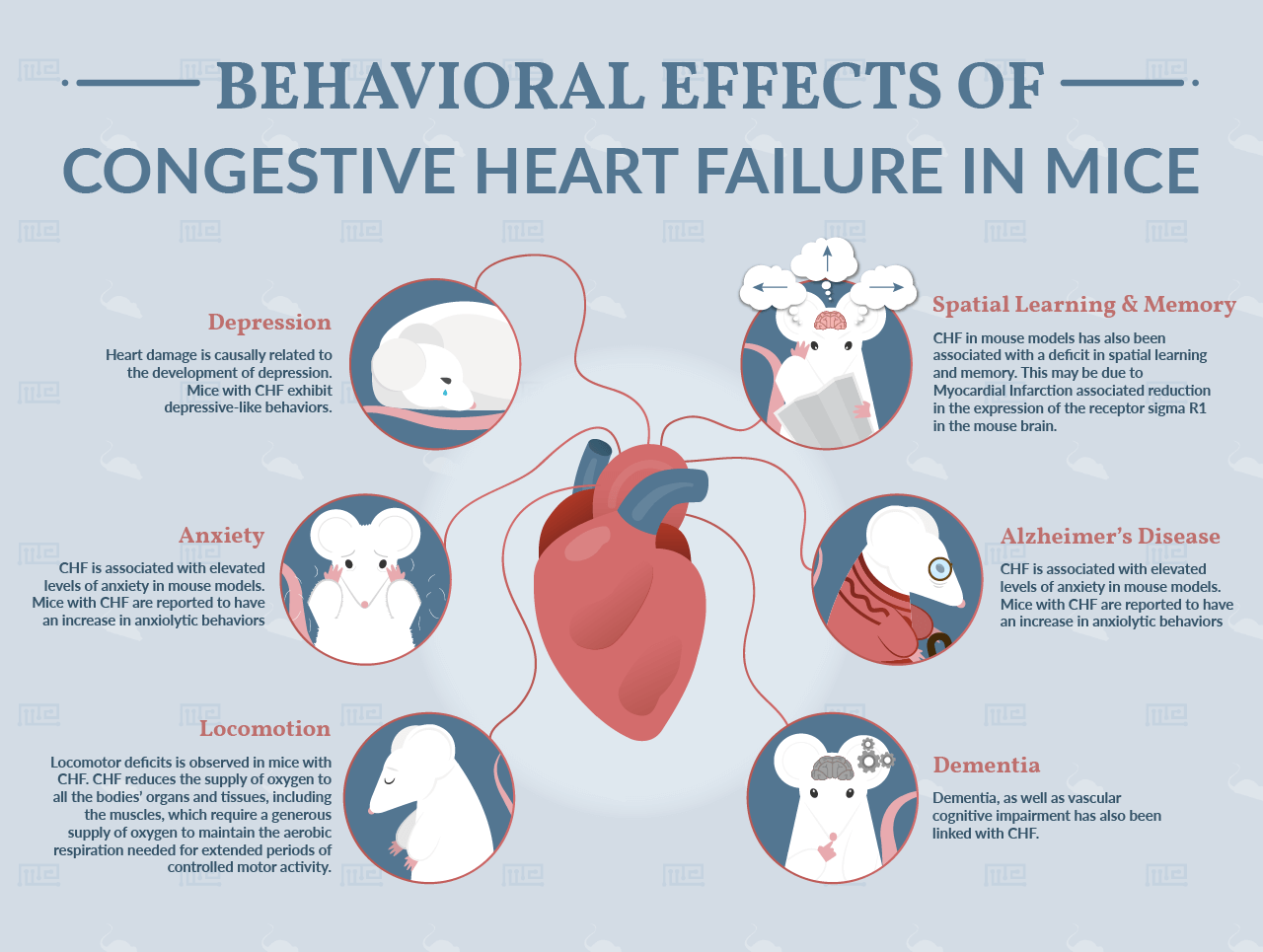
Since the brains of both humans and mice are intimately connected with all the body’s organ systems, diseases affecting bodily organs can also have neurological and behavioral implications. CHF and MI are no exception. In particular, experimental observations have associated these disorders with a range of cognitive and behavioral phenomena, including depression, anxiety, dementia and deficits in locomotion and spatial memory. In this article, we will discuss these behavioral consequences of MI and CHF.
CHF and Depression
A study conducted in Germany in 2014 observed a marked depressive effect in mice with CHF induced by MI.[3] The CHF mice appeared to experience “anhedonia”, a decreased capacity to experience pleasure, as shown by their reduced intake of sucrose compared to control mice. The worse the damage to each mouse’s heart tissue, the stronger the observed reduction in its sucrose intake. The CHF mice were also less motivated and exhibited significantly less movement.
Similar results came from a Japanese study published in 2016.[4] Following a marked reduction in blood flow through the aorta, mice experienced heart failure and then exhibited what the researchers described as “depressive-like behaviors”. The CHF mice moved significantly less than controls in a forced swimming task in which each mouse is placed into water (a displeasing environment for a mouse), and also struggled less when suspended by their tails. This study also replicated the German researchers’ observation[3] that CHF mice engage in reduced sucrose consumption.
A 2017 study reported depression-like behaviors in a mouse model of hypertrophic cardiomyopathy.[5] While this condition differs from CHF, it is interesting to note that other conditions involving reduced heart function have also been associated with depression. The evidence of this study strengthens the inference that heart damage per se is causally related to the development of depression. Rather strangely, depressive behavior in this study was only seen in female mice, and hence hormonal factors may also make a major contribution to the pathology in this instance.
CHF and Anxiety
The German study from 2014 also assayed the CHF mice for anxiety associated behaviors.[3] Interestingly, the researchers inferred that CHF was associated with elevated levels of anxiety in these mouse models, as shown by their performance in the elevated plus maze and the light-dark box test.
In the elevated plus maze, mice are placed in the middle of a plus-shaped platform that is positioned a certain distance from the ground. The maze has closed arms as well as arms exposed to the open air; mice that spend more time on the closed than open arms, as the CHF mice did in this study, are considered to have elevated levels of anxiety.
The light-dark box test has a similar set-up. In this case, mice are placed in a box with two compartments: a lit compartment, and a covered compartment in complete darkness. Greater time spent by mice hiding in the dark portion of the box as opposed to exploring the lit portion is interpreted as a sign of anxiety. It is worth bearing in mind that some scientists have questioned the reliability of the light-dark box test,[6] arguing that it does not correctly assay anxiety under some circumstances.
This German study corroborates the results of a Chinese study from 2013,[7] which also found decreased willingness of CHF mice to venture out onto the arms of the elevated plus maze. It is important to bear in mind that these anxiety assays rely on the observation of movement, which may also be affected by locomotor deficits (as discussed in the next section of this article).
However, it is important to note that the 2017 study[5] focusing on hypertrophic cardiomyopathy (the same study mentioned above associating this condition with depressive behavior) also reported an increase in anxiolytic behaviors compared to controls. Thus, it seems cardiac conditions per se can indeed have anxiolytic effects not mediated by locomotor deficits. Why heart conditions should result in increased anxiety in mice remains somewhat of a mystery.
CHF and Locomotion
Since both depression and anxiety are assessed in mouse models using a number of tests where behaviors that involve movement (such as the forced swimming test, the elevated plus maze etc) are central, it can be difficult to tease apart mood disorders from disorders of locomotion. If a CHF mouse moves less than controls during a forced swimming test, does this mean that CHF is thus associated with depression, with motor deficits, or both?
The results mentioned above, where less movement away from the center of the elevated plus maze by CHF mice was interpreted as elevated anxiety, could also be explained by a motor deficit where the mice are unable to move as well as controls. The same ambiguity arises when considering the “depressive-like behaviors” displayed by mice in the forced swimming test in the Japanese study from 2016.
A test which is more specific to motor deficits than to psychological states, and which might help to tease apart effects of CHF on locomotion from its potential depressive or anxiolytic effects, is the rotarod. In this test, mice which fall down more rapidly than controls from a rotating cylinder are said to have reduced motor capabilities. And indeed, a study from 2016 did show a diminished performance by CHF mice on the rotarod test.[9] This evidence strengthens the case for the presence of particular locomotor deficits in mice with CHF.
Upon reasoned consideration, it is not surprising that CHF is associated with reduced capacity for dexterous movement. CHF reduces the supply of oxygen to all the bodies’ organs and tissues, including the muscles, which require a generous supply of oxygen to maintain the aerobic respiration needed for extended periods of controlled motor activity. Explaining why CHF affects mood seems more challenging, and separating pure depressive and anxiolytic effects of the disorder from its motor effects may require new experimental paradigms.
CHF and Spatial Learning & Memory
CHF in mouse models has also been associated with a deficit in spatial learning and memory. A 2017 study[10] reported significantly worse performance in the Morris water maze test by mice with CHF following surgically induced MI. In this test, mice must remember the location of an elevated platform that allows them to escape from a circular pool of water. The same study also reported deficits in a different form of memory, as evidenced by a diminished performance of the CHF mice in an object recognition task.
Reduced performance in the Morris water maze by CHF mice was also reported by the Chinese study published in 2013.[7] A study from the same year,[8] this time undertaken by Japanese researchers, reports reduced performance by MI model mice in the Y maze test (a test in which control mice preferentially explore parts of the maze they do not remember visiting before). Furthermore, the Japanese researchers offer a molecular biological explanation for the memory deficit: an MI associated reduction in the expression of the receptor sigma R1 in the mouse brain.
In both humans and mice, the hippocampus is the part of the brain primarily linked with capacity for spatial navigation, learning and memory. Studies in humans have shown damage and structural abnormalities in the hippocampus following CHF.[11] Such structural abnormalities have not been investigated in the brains of mouse models, but are likely to be present and to contribute to the diminished performance of CHF mice in spatial memory tests.
Congestive Heart Failure and Alzheimer’s Disease
Since the brain needs a constant and plentiful supply of blood in order to maintain optimal functionality, it is not surprising that the loss of blood pressure associated with CHF is associated with various forms of cognitive decline. It is however perhaps a little surprising that CHF has also been linked with the development of neurodegenerative disorders primarily associated with the aggregation of misfolded, cytotoxic proteins.
There is some experimental evidence for a causal link between CHF and the development of Alzheimer’s Disease (AD). Mice cannot contract AD, but mouse models of the condition have been created and used in AD research. The Chinese study from 2013[7] showed alterations in the metabolism of beta amyloid, one of the proteins which when misfolded and aggregated is believed to underlie neuronal death in AD. As mentioned above, this study also reported spatial learning deficits in the CHF mice, consistent with the memory loss normally seen in human AD patients.
Several other studies have also reported apparent connections between CHF and AD-like pathology in mice. A 2009 study from Italy[12] using mice with CHF induced by aortic ligation found that these mice showed greater deposition of beta amyloid in the cortex compared to controls. Greater amyloid protein deposition was also seen by a group of Japanese researchers using a very similar mouse model, with results published in the same year.[13]
Congestive Heart Failure and Dementia
Most recently, a 2018 study from Poland using mice with CHF induced by expression of the signaling protein Gaq*44 found a link between heart failure and vascular cognitive impairment.[14] Vascular cognitive impairment refers to a reduction in cognitive capacity resulting from insufficient blood flow to the brain, and is a less severe form of vascular dementia.
Conclusion
It is clear from the various studies mentioned in this article that myocardial infarction and subsequent congestive heart failure can have a profound effect on mouse behavior. The research detailed here has presented evidence for a causal relationship between CHF and depression, anxiety, dementia, and deficits in both locomotor activity and spatial learning and memory. These experimental results add to a growing awareness of how disorders affecting organs beyond the brain can have neurological and behavioral consequences. Hopefully, in the future, this knowledge will allow us to better understand and treat MI and CHF pathology in human patients.
References
- CDC, NCHS. Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released 2015.
- Schocken DD1, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol. 1992 Aug;20(2):301-6.
- Anna Frey, Sandy Popp, Antonia Post, Simon Langer, Marc Lehmann, Ulrich Hofmann, Anna-Leena Sirén, Leif Hommers, Angelika Schmitt, Tatyana Strekalova, Georg Ertl, Klaus-Peter Lesch and Stefan Frantz. Experimental heart failure causes depression-like behavior together with differential regulation of inflammatory and structural genes in the brain. 2014. Behav. Neurosci. 8:376.
- Yasuharu Shinoda , Hideaki Tagashira , Md. Shenuarin Bhuiyan, Hideyuki Hasegawa, Hiroshi Kanai, Chen Zhang, Feng Han, Kohji Fukunaga. Corticosteroids Mediate Heart Failure-Induced Depression through Reduced σ1-Receptor Expression. 2016. PLoS ONE 11(10).
- Amanda M. Dossat, Marcos A. Sanchez-Gonzalez, Andrew P. Koutnik, Stefano Leitner, Edda L. Ruiz, Brittany Griffin, Jens T. Rosenberg, Samuel C. Grant, Francis D. Fincham, Jose R. Pinto, and Mohamed Kabbaj. Pathogenesis of depression- and anxiety-like behavior in an animal model of hypertrophic cardiomyopathy. 2010. report of a Working Group of the National Heart, Lung, and Blood Institute.
- Ennaceur, A. Tests of unconditioned anxiety — Pitfalls and disappointments. 2013. Physiology & Behavior. Volume 135, August 2014, Pages 55-71.
- Xiaoqi Hong , Liping Bu , Yi Wang , Jing Xu , Jian Wu , Yufang Huang, Jie Liu, Haiyun Suo, Lumeng Yang, Yuncen Shi, Yi Lou, Zhengliang Sun, Guoqi Zhu, Thomas Behnisch, Mei Yu, Jianguo Jia, Wangxi Hai, Hongping Meng, Sheng Liang, Fang Huang , Yunzeng Zou , Junbo Ge. Increases in the Risk of Cognitive Impairment and Alterations of Cerebral β-amyloid Metabolism in Mouse Model of Heart Failure. PLoS ONE 8(5): e63829.
- Ito K1, Hirooka Y, Sunagawa K. Brain sigma-1 receptor stimulation improves mental disorder and cardiac function in mice with myocardial infarction. 2013. J Cardiovasc Pharmacol. 2013 Aug;62(2):222-8.
- Aline V.N. Bacurau, Paulo R. Jannig, Wilson M.A.M. de Moraes, Telma F. Cunha, Alessandra Medeiros, Laura Barberi, Marcele A. Coelho, Reury F.P. Bacurau, Carlos Ugrinowitsch, Antonio Musarò, Patricia C. Brum. Akt/mTOR pathway contributes to skeletal muscle anti-atrophic effect of aerobic exercise training in heart failure mice. Journal Cardiology. July 1, 2016. Volume 214, Pages 137–147.
- Hay, M., Vanderah, T. W., Samareh-Jahani, F., Constantopoulos, E., Uprety, A. R., Barnes, C. A., & Konhilas, J. (2017). Cognitive impairment in heart failure: A protective role for angiotensin-(1-7). Behavioral Neuroscience, 131(1), 99-114.
- Woo MA, Ogren JA, Abouzeid CM, et al. Regional Hippocampal Damage in Heart Failure. European journal of heart failure. 2015;17(5):494-500.
- Gentile MT1, Poulet R, Di Pardo A, Cifelli G, Maffei A, Vecchione C, Passarelli F, Landolfi A, Carullo P, Lembo G. Beta-amyloid deposition in brain is enhanced in mouse models of arterial hypertension. Neurobiol Aging. 2009 Feb;30(2):222-8.
- Kitaguchi H1, Tomimoto H, Ihara M, Shibata M, Uemura K, Kalaria RN, Kihara T, Asada-Utsugi M, Kinoshita A, Takahashi R. Chronic cerebral hypoperfusion accelerates amyloid beta deposition in APPSwInd transgenic mice. 2009. Brain Res. 2009 Oct 19;1294:202-10.
- Mateusz G. Adamski, Magdalena Sternak, Tasnim Mohaissen, Dawid Kaczor, Joanna M. Wierońska, Monika Malinowska, Iwona Czaban, Katarzyna Byk, Kristina S. Lyngsø, Kamil Przyborowski, Pernille B.L. Hansen, Grzegorz Wilczyński, Stefan Chlopicki. Vascular Cognitive Impairment Linked to Brain Endothelium Inflammation in Early Stages of Heart Failure in Mice. 2018. Journal of the American Heart Association. vol. 7 no. 7 e007694.